New Frontiers in Team Science: Empowering Patients With AI-Driven E-Consults
#Methods
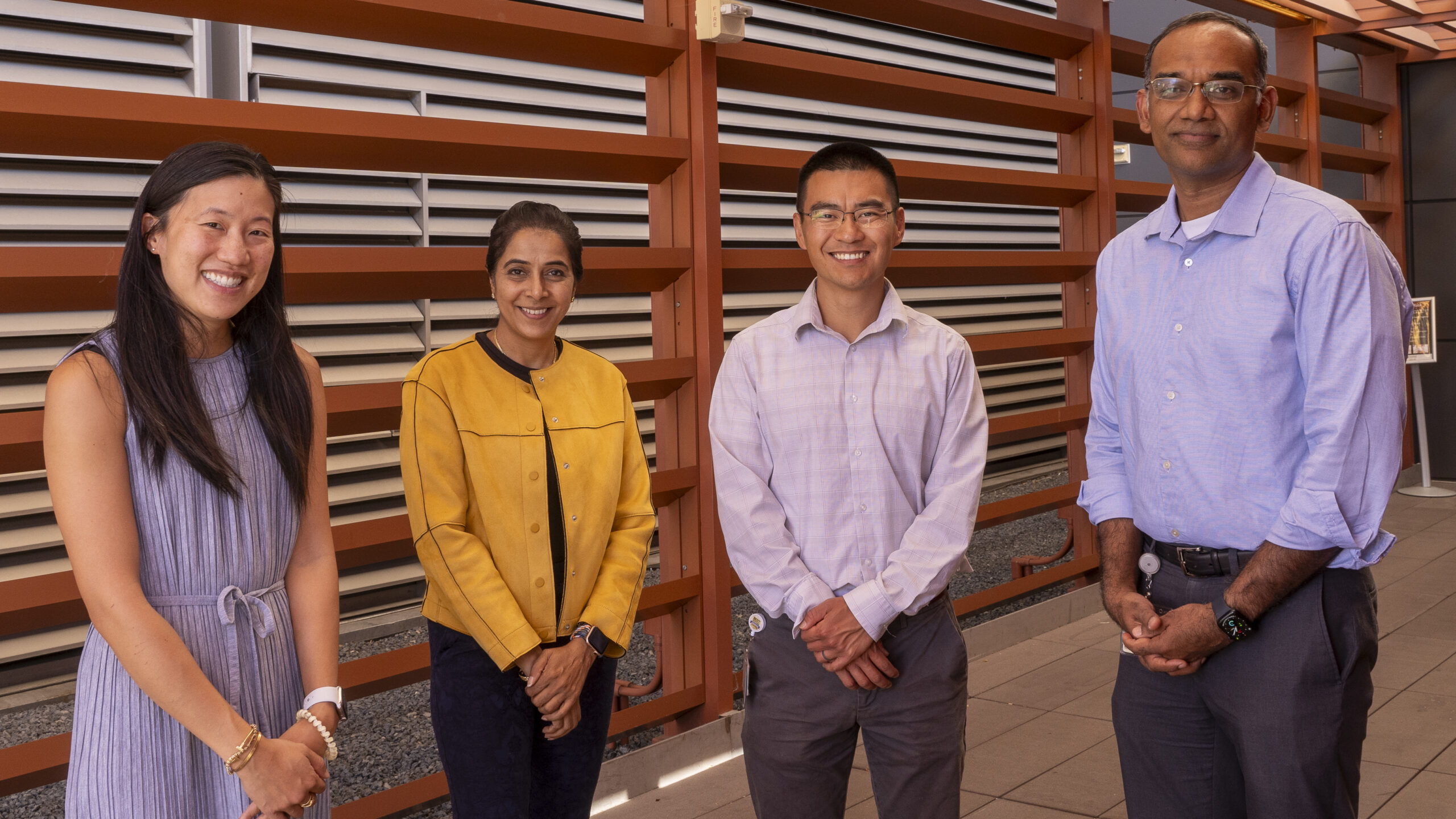
From left: Olivia Jee, MD; Vijaya Parameswaran, PhD; Ron Li, MD; and Srikanth Muppidi, MD
For patients with rare diseases, the time to obtain a definite diagnosis can be months or even years. During that period, even minor communication gaps can lead to dead ends and lengthen the journey. Here is a typical scenario:
Patient A goes to see their primary care physician complaining of diffuse symptoms that have plagued them for some time. The physician suspects a neurological disorder and initiates what is known as an e-consult – a digital, physician-to-physician communication. The patient’s symptoms are described in medical shorthand, including numerous acronyms and technical terms. The consulted neurologist suggests a series of tests, which are ordered and performed in the following days and weeks, all with negative or inconclusive results.
The primary care physician refers the patient for an in-person visit to the neurologist, who is not available for some months. When that date finally arrives, the neurologist consults the notes received and discusses them with the patient. The patient clarifies one particular symptom as well as its timing: “No, that is incorrect. Here’s what actually happened…”
That clarification serves as a clue, and after a careful examination and more questions, the neurologist confirms the diagnosis of a rare disease, at which point the patient is put on appropriate medication. The time from initial visit to treatment: several months, during which the patient’s condition has worsened.
Patient A knew how to access the physician’s notes and the response from the neurologist. But the medical terminology and the acronyms used obscured the fact that there was a miscommunication about one crucial symptom and its timing, which then led to a series of mistaken assumptions.
What if an AI tool could serve as an interpreter to translate physicians’ notes into lay language? What if patients could easily access this translation and directly respond with corrections or additional details?
These questions will be explored in a new pilot study at Stanford. In an example of true team science, the project brings together professionals from different fields. Primary care physicians, neurologists, and experts in AI tools for medicine will investigate how patients communicate with their care team and how they could be active participants when their primary care physician consults a specialist.
“Timely communication is essential in healthcare delivery. We are exploring whether the integration of large language models can augment human clinical care by improving the efficiency and effectiveness of patient communication,” says Vijaya Parameswaran, PhD, a social scientist in the Division of Cardiology and co-principal investigator of the study. Large language models, she explains, are the foundation for chatbots like ChatGPT – computer programs that simulate and process human conversation, either written or spoken.
The research will also study how physicians consult with each other and with their patients during an e-consult to see if artificial intelligence language models can improve these interactions and information sharing.
“The time it takes the primary care physician to formulate a tight, well supported clinical question and the specialist’s time providing a clinical assessment and recommendations impact the quality and quantity of e-consults. If AI can aid to overcome these barriers, it will help us continue to grow the program and provide more efficient clinical care,” says Olivia Jee, MD, a primary care physician, clinical assistant professor of primary care and population health, and medical director of the Stanford Health Care eConsult Program.
“Timely communication is essential in healthcare delivery. We are exploring whether the integration of large language models can augment human clinical care by improving the efficiency and effectiveness of patient communication,” says Vijaya Parameswaran, PhD
For example, an AI language tool could be used by a specialist to quickly scan and condense what is often hundreds of pages of history and data that patients with rare diseases typically bring to a consultation. The most brilliant human minds do not have the capacity to digest thousands of pieces of information in a few minutes and come to rational conclusions. A large language model tool can serve as an “extra brain” to sift through the data, bring the most relevant facts into focus, and suggest the most likely diagnosis and possible treatments, according to Srikanth Muppidi, MD, clinical professor of neurology and neurological sciences and co-investigator in the study.
“With the increasing complexity of care and silos of knowledge, it is impossible for primary care or referring physicians to always obtain and interpret relevant clinical information. This study will help us understand how best to use AI tools to review referrals, both to reduce the time to diagnosis and to help choose the best therapy for each individual,” says Srikanth Muppidi, MD.
On the patient side, the same tools could empower them with language and technological resources that would help them communicate about their symptoms and disease history. A rare disease forces patients on a journey from primary care to specialists to subspecialists, each time having to explain the course of their condition, pointing out tests that have been administered, and describing the effects of attempted treatments. By making it easier for patients to be actively involved in the process of diagnosis and disease management, the Stanford team hopes to shorten these difficult journeys and improve outcomes for patients.
The study is a joint project of the Stanford Department of Medicine Team Science program, the Stanford Health Care Digital Healthcare Integration Team, and UCB Biopharma, the industry sponsor.
“Large language models have shown tremendous promise in improving clinical workflows by helping to summarize and translate information,” says Ron Li, MD, a clinical associate professor of medicine and medical informatics director for digital health, who is the principal investigator of the study. “The goal of this project is to explore how we can apply this capability to enable and transform care models such as e-consults while keeping patients at the center.”

Social Scientist in Cardiovascular Medicine Vijaya Parameswaran, PhD
