Cutting-Edge Science Delivers Insights Into the Inner Workings of Autoimmune Diseases
#Methods
Suzanne Tamang, PhD; PJ Utz, MD; and Titilola Falasinnu, PhD
Autoimmune and rheumatic diseases can impact anyone, often affecting individuals in the prime of their lives—during their 20s, 30s, and 40s. The consequences not only are personal, as these conditions can disable the most active members of our society, but also have profound societal impacts. Families are burdened, and economic productivity is lost. Despite this significant impact, these diseases remain some of the most misunderstood and neglected areas in medicine.
“The challenges we face in understanding and managing autoimmune and rheumatic diseases are substantial. Yet, they are not insurmountable,” says Bill Robinson, MD, PhD, professor and division chief of immunology and rheumatology. “With the convergence of computational power and biomedical expertise, we are now poised to unravel these complexities.”
In the Division of Immunology and Rheumatology, three pioneering researchers – Suzanne Tamang, PhD, PJ Utz, MD, and Titilola Falasinnu, PhD – are at the forefront of an exciting scientific frontier. They are using cutting-edge computational and informatics techniques to redefine our understanding and management of autoimmune and rheumatic diseases.
“Better understanding the mechanisms underlying autoimmune rheumatic diseases will provide insights that will lead to the development of next-generation therapeutics with the potential to provide more effective and fundamental treatment, thereby enabling people with autoimmune diseases to live healthy, productive, and vibrant lives,” Robinson says.
Synthetic Patients Help Uncover Environmental Impacts on Autoimmune Diseases
Assistant Professor Suzanne Tamang, PhD, is unleashing the latest in AI technologies with a rich and vast veteran database to better understand the effects of environmental factors such as air pollution on autoimmune disorders and rheumatic diseases.
Through her work with the Department of Veterans Affairs medical database, Tamang has developed a natural language processing system that analyzes over a million patient notes daily, extracting important risk factors previously locked up in unstructured text. This information helps the VA better address the complex needs of veterans nationwide.
Tamang is also creating “synthetic populations” with her collaborators at the start-up MDClone to enable new studies on the environmental triggers of autoimmune disorders and rheumatic diseases like rheumatoid arthritis. By anonymizing real patient data and linking it to environmental exposures, Tamang aims to understand disease flares and improve patient outcomes.
“They are synthetic patients,” Tamang says of the AI-created population. “It was derived from real veterans, although it’s synthetic. It’s a new method, based on generative AI, and it allows us to bring in environmental data to explore different ways to link it to population health.”

Professor Suzanne Tamang, PhD, applies cutting-edge AI to veteran data to uncover how environmental factors like air pollution affect autoimmune and rheumatic diseases.
“‘They are synthetic patients,’ Suzanne Tamang, PhD, says of the AI-created population. ‘It was derived from real veterans, although it’s synthetic. It’s a new method, based on generative AI, and it allows us to bring in environmental data to explore different ways to link it to population health.’”
Tamang’s population health approach considers how the interplay of clinical, social, and environmental factors influences health outcomes. Her research using air pollution data from the U.S. could help clinicians mitigate flares caused by factors like wildfire smoke.
The synthetic population, encompassing a diverse range of demographics and geographic locations across the U.S., not only enhances the generalizability of her findings but also maintains patient privacy. This innovative method supports the development of predictive models that could significantly improve healthcare responses to environmental triggers.
Tamang’s work advances autoimmune research by translating complex AI technologies into practical tools that improve access to quality health care for vulnerable populations. Her pioneering efforts aim to empower health systems with data to better anticipate and mitigate the impacts of environmental factors on health outcomes.
“Our work aims to unite various experts to tackle these significant challenges by providing them with comprehensive datasets,” she says. “This approach marks a critical advancement in our ongoing projects within the new climate and health space.”
Massive Scale of COVID-19 Unlocks New Insights Into Autoimmune Responses
In a significant shift in understanding autoimmune diseases, PJ Utz, MD, professor of immunology and rheumatology, leads Stanford’s research efforts to leverage the unprecedented scale of COVID-19 to reveal how the virus may initiate long-term autoimmune processes.
Utz and his team are using advanced technology to study thousands of proteins at once, helping them understand the complex immune system issues in long COVID-19. Their research has found that some COVID-19 patients develop autoantibodies, which are proteins that mistakenly attack the body. This supports the idea that the virus can trigger autoimmune diseases. These findings, driven by the widespread effects of the pandemic, are leading doctors to rethink how they approach the treatment and understanding of infectious diseases and autoimmunity.
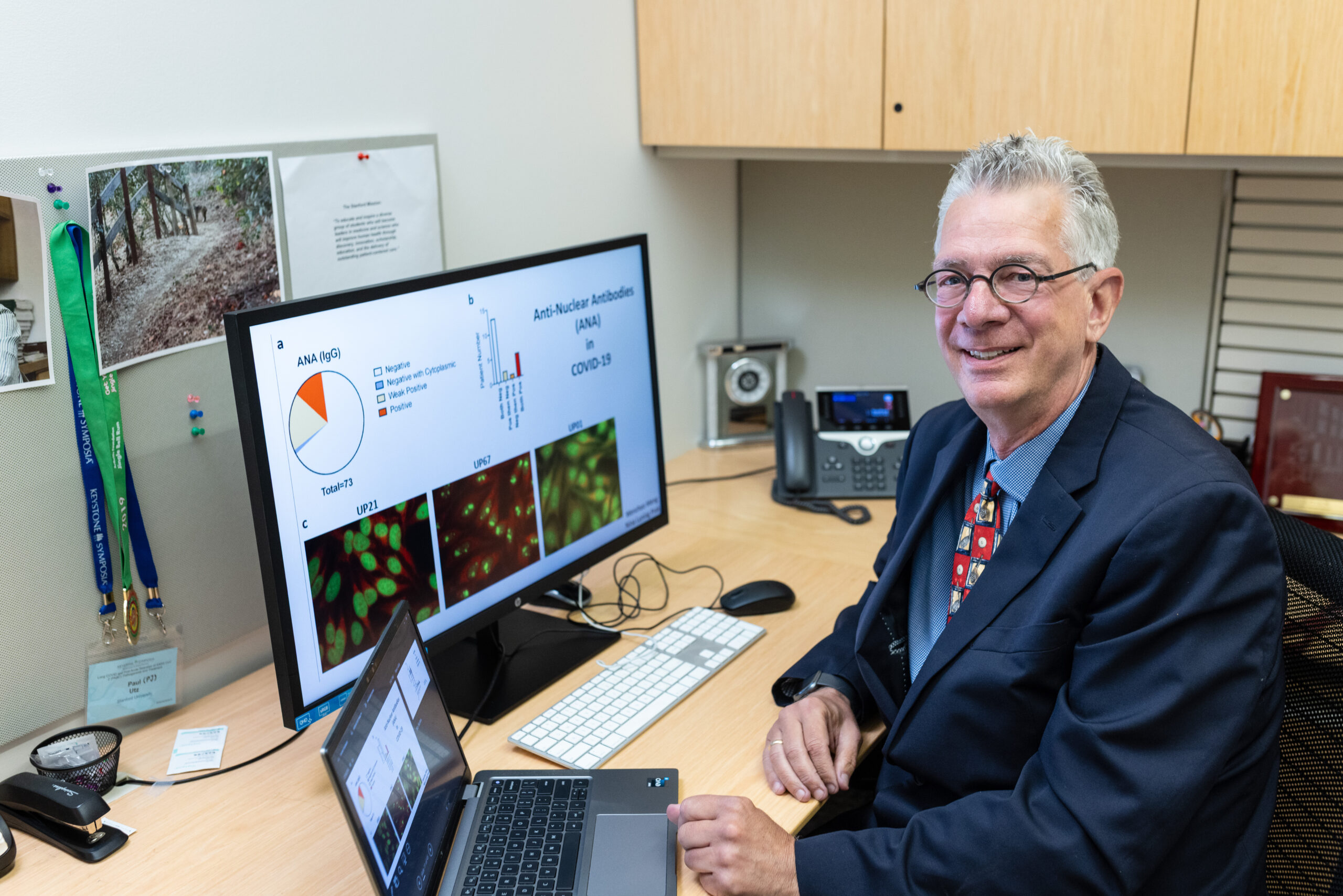
Leading a groundbreaking exploration of post-viral autoimmunity, PJ Utz, MD, harnesses the massive scale of COVID-19 to unravel hidden complexities of the autoimmune response.
“We have such a unique opportunity here with this pandemic that I’ll spend the rest of my career studying how COVID-19 triggers autoimmunity and how we can treat it.”
– PJ Utz, MD
When the pandemic began, Stanford and other institutions proactively started to collect samples, enroll patients, and study the disease as it evolved.
“We were essentially building the new immunological frontier while the airplane was being built,” Utz explains. This proactive approach has allowed researchers to capture unprecedented data on the immune responses triggered by COVID-19.
Building on the knowledge gained from past pandemics, today’s researchers, equipped with unparalleled clinical samples and molecular tools, are now able to conduct detailed studies of viral effects on the immune system and advance theories about post-viral autoimmune effects that were previously speculative.
“We have such a unique opportunity here with this pandemic,” Utz says, “that I’ll spend the rest of my career studying how COVID-19 triggers autoimmunity and how we can treat it.”
New Research Offers Solutions and Hope for People With Chronic Pain
Motivated by helping individuals with chronic pain, Titilola Falasinnu, PhD, assistant professor of immunology and rheumatology, is dedicated to developing innovative methods to alleviate the suffering of patients with autoimmune rheumatic diseases. Her work aims to enhance daily living and improve quality of life by addressing pain that often impairs everyday activities.
Despite treatment advances in rheumatology, pain remains the most prominent, unaddressed patient complaint. Depending on the diagnosis, upwards of 65% of patients are on long-term opioid therapies and have higher rates of opioid overdose hospitalizations than the general population, Falasinnu says.
“Given these significant burdens, there is a critical need for innovative research to develop better pain management strategies and improve patient outcomes,” she says. “It is imperative to study pain not just as a symptom but as a disease in its own right to understand its impact better and develop effective treatments.”

Dedicated to reducing opioid dependence and enhancing the quality of life for people with autoimmune diseases, Titilola Falasinnu’s research paves the way for personalized treatments that address both biological and psychosocial factors.
“Our research not only advances our understanding of chronic pain and autoimmune diseases but also transforms patient care through personalized medicine and predictive modeling, shaping future public health strategies.”
– Titilola Falasinnu, PhD
The Falasinnu Lab is composed of epidemiologists, clinicians, pain scientists, and informaticists who use large datasets and advanced computational methods to understand the complex nature of pain in patients with autoimmune rheumatic diseases, such as lupus. They are developing predictive models to forecast pain episodes in patients to enable personalized medicine and treatment plans.
Their research has illuminated overlapping factors that influence chronic pain, paving the way for interventions that address both biological and psychosocial aspects of pain management. The aim is to improve patient quality of life and reduce reliance on long-term opioid therapies, which carry significant health risks.
“Our research not only advances our understanding of chronic pain and autoimmune diseases but also transforms patient care through personalized medicine and predictive modeling, shaping future public health strategies,” she says.
