Lung Organoids: A Novel Way to Model COVID Infection
A year into the pandemic, we’ve all heard the stories. A patient is a little short of breath but appears to have a mild case of COVID-19. The next day, she deteriorates so rapidly that she’s rushed to intensive care, put on a ventilator, and hooked up to a dialysis machine to prevent kidney failure. Her overzealous immune system has gone rogue, attacking healthy cells instead of just fighting off the virus.
What triggers this devastating immune response, called a cytokine storm? Researchers are still struggling to identify the underlying processes that initiate a COVID infection and subsequent cytokine storm.
Biologists use advanced technologies and cell cultures in petri dishes to study severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the coronavirus strain responsible for COVID-19, identifying its key characteristics such as the famous crownlike spikes on their surfaces. But these short-lived cultures don’t act like real organs. And scientists are limited by their samples.
“When you analyze samples from patients, they’re often at the end stage of the disease, and many of the samples are from autopsy. You can’t understand the initiation process because the tissue is essentially destroyed,” says Calvin Kuo, MD, PhD, professor of hematology.
Understanding how the disease develops and testing potential treatments require better ways to model this coronavirus.
Miniature Organs in a Dish
Kuo’s laboratory develops organoids—three-dimensional miniature organs grown in a petri dish that mimic the shape, structure, and tissue organization of real organs.
Grown from human tissue samples using precisely defined ingredients, these organoids are little spheres of gel up to 1 millimeter in diameter. Healthy tissue samples are mechanically minced and enzyme digested to get to single cells, and then the organoids are grown from single stem cells. They last about six months, significantly longer than the few-weeks lifetime of traditional cell cultures.
Kuo initially developed organoids to study stem cell biology and model cancer. His team was the first to use organoids to convert normal tissues to cancer, as previously reported in Nature Medicine.
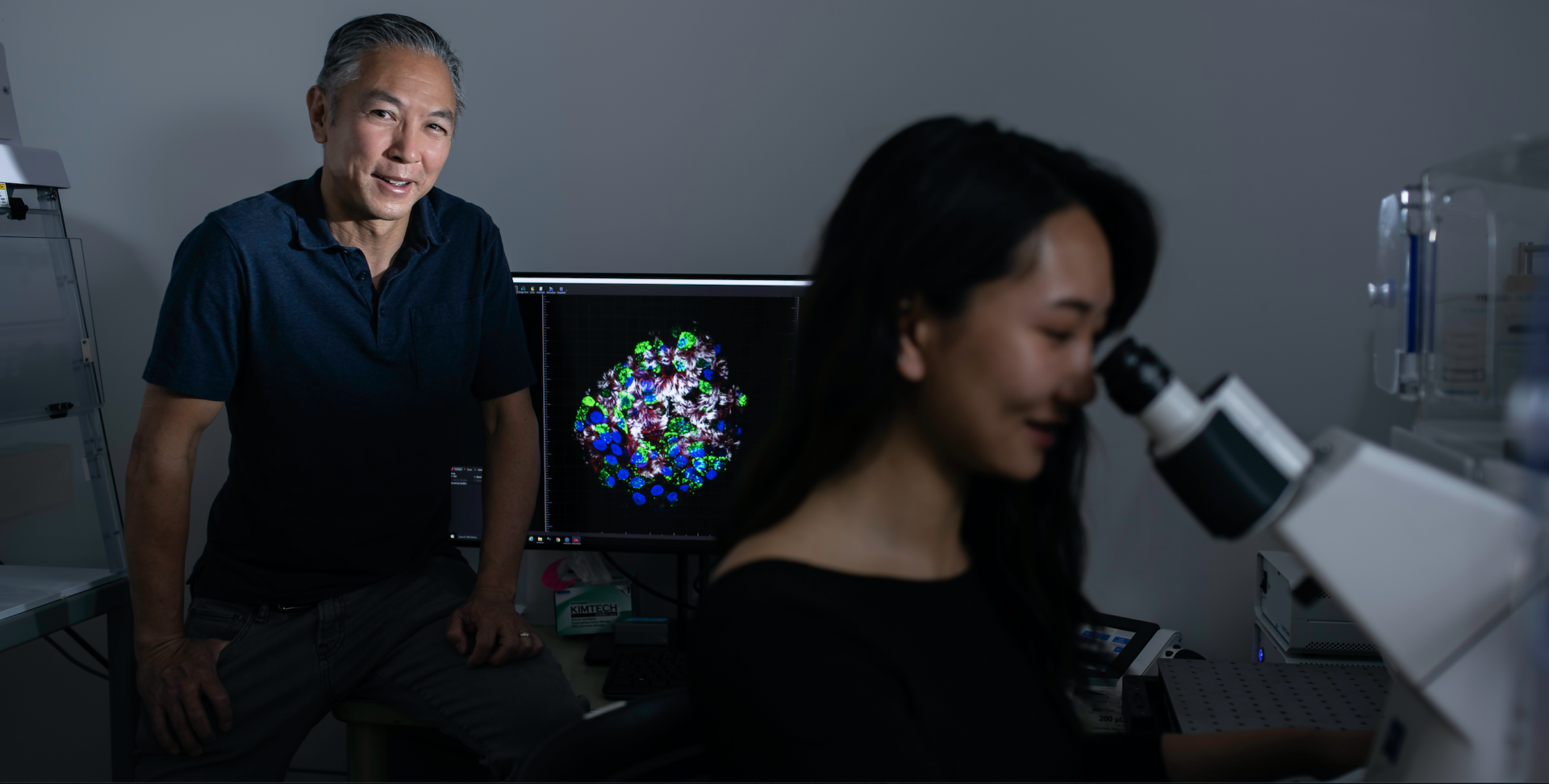
Calvin Kuo, MD, PhD, with Shannon Choi, MD, PhD, a student in the Kuo lab. Courtesy Steve Fisch
But he was passionate about using organoids to model infectious diseases. In 2015, he led a National Institute of Allergy and Infectious Diseases U19 research program, recently renewed for an additional five years, in collaboration with Stanford researchers Manuel Amieva, MD, professor of pediatrics and of microbiology and immunology; Harry Greenberg, MD, the Joseph D. Grant Professor in the Stanford University School of Medicine and professor of microbiology and immunology; Elizabeth Mellins, MD, professor of pediatrics; and Sarah Heilshorn, PhD, professor of materials science and engineering. Focusing mainly on the gastrointestinal tract, this multidisciplinary team provided proof of principle that organoids could model infectious diseases.
“With an organoid system, you can start at the infection and look at the very earliest events that occur after infection. And those can give insights as to what needs to be blocked therapeutically,” Kuo explains.
Distal Lung Organoids
After the initial success with gastrointestinal organoids, Ameen Salahudeen, MD, PhD, a hematology and oncology postdoctoral fellow working in Kuo’s lab, led efforts to expand this work by developing distal lung organoids. He partnered with lung stem cell expert Tushar Desai, MD, associate professor of pulmonary, allergy, and critical care medicine at Stanford.
The distal lung is composed of terminal bronchioles and alveolar air sacs, where inhaled air passes through the tiny ducts from the bronchioles into the elastic air sacs. It performs essential respiratory functions that can be compromised by inflammatory or infectious disorders, such as COVID-19 pneumonia.
“Growing distal lung cultures in a pure way that doesn’t require any supporting feeder cells and is in a chemically defined media had not been possible,” Kuo says. “We were able to do this very beautifully—to grow alveoli at the terminal bronchioles as long-term human cultures.”
The team developed two types of distal lung organoids. Both were made from human distal lung samples provided by Stanford cardiothoracic surgeon Joseph Schrager, MD.
They grew the first type, alveolar organoids, from single alveolar type 2 (AT2) stem cells. AT2 cells have several important functions that together help control the immune response to decrease lung injury and repair. The scientists then induced the AT2 cells to produce alveolar type 1 (AT1) cells, which are the thin-walled cells lining the alveolar air sacs; they are essential for the lung’s gas-exchange function.
“The second type are the basal organoids, which grow from single basal stem cells. They give rise to the mucus-secreting club cells and the ciliated cells with beating hair. And we can see the beating hair under the microscope—it’s quite dramatic,” describes Kuo. “That’s a very nice reproduction of the differentiation and function of the lung.” The team also grows a mixture of alveolar and basal organoids.
They selected these organoid types to determine which cell types in the bronchioles and alveoli were infectible—in hopes of identifying the different mechanisms for how viruses cause respiratory compromise.
Initially, they tested the distal lung organoids using the H1N1 influenza virus, collaborating with Stanford molecular virology expert Jeff Glenn, MD, PhD.
The team fluorescently labeled the virus and infected the lung organoids, demonstrating that the virus replicated in both basal and alveolar organoids. Next, they did more sophisticated PCR-based testing to show that the virus replicated its genome.
COVID-19 Model
“But then the COVID-19 pandemic hit, so we initiated a fabulous collaboration with infectious disease expert Catherine Blish, MD, PhD, in the Department of Medicine, to infect our lung organoids with SARS-CoV-2. This was driven by a talented MD-PhD student in my lab, Shannon Choi,” says Kuo. “She worked with Arjun Rustagi, an infectious disease fellow in Catherine Blish’s lab, who infected the organoids in a biosafety-level-3 lab.”
Another partnership was critical, though. An important coronavirus receptor, called angiotensin-converting enzyme 2, or ACE2, resides inside the lung organoids. But ACE2 needed to be on the outside of the organoid to get the infection going.
“We discovered an unknown basal cell
subpopulation containing the stem cell activity.
And then we showed this subpopulation
actually existed in human lungs in very
interesting anatomic locations”
“We discovered an unknown basal cell
subpopulation containing the stem cell activity.
And then we showed this subpopulation
actually existed in human lungs in very
interesting anatomic locations”
Luckily, Amieva previously devised a way to flip intestinal organoids inside out. Working together, Choi and Amieva turned the lung organoids inside out.
As reported in Nature in November 2020, the team demonstrated that the coronavirus infected their distal lung organoids, including the alveolar air sacs, where COVID-19 pneumonia originates. They also identified a new airway subpopulation as a COVID-19 virus target cell.
“Everyone knew basal cells were stem cells in the lung, but they thought they were all equivalent. Using our organoids, we discovered an unknown basal cell subpopulation containing the stem cell activity. And then we showed this subpopulation actually existed in human lungs in very interesting anatomic locations,” Kuo says.
COVID-19 Applications
According to Kuo, their distal lung organoids have three major applications for COVID-19.
They are using them to screen potential coronavirus therapeutic antibodies and to understand how these treatments work. Although initially focused on COVID-19, this screening will likely expand to other kinds of lung infections in the future.
Because the distal lung with the alveoli is the site of the COVID-19 pneumonia, they also plan to use the organoids to identify the underlying biological mechanisms behind coronavirus infection. Finally, they plan to extend their organoid system to incorporate immune cells and understand more complex processes. In particular, they plan to model the dreaded cytokine storm.
Overall, Kuo emphasizes that this organoid research represents a huge team effort involving many investigators with wide-ranging expertise from various departments at Stanford, as well as an “interesting evolution of events.”
“Now we have a human experimental system to model SARS-CoV-2 infection of the distal lung with alveoli, which is the site of the lung disease that kills patients,” he summarizes. “We know patients die because of severe pneumonia and lung failure. We can now recapitulate this in the dish. So, we can study how it works, and also test drug treatments.”
