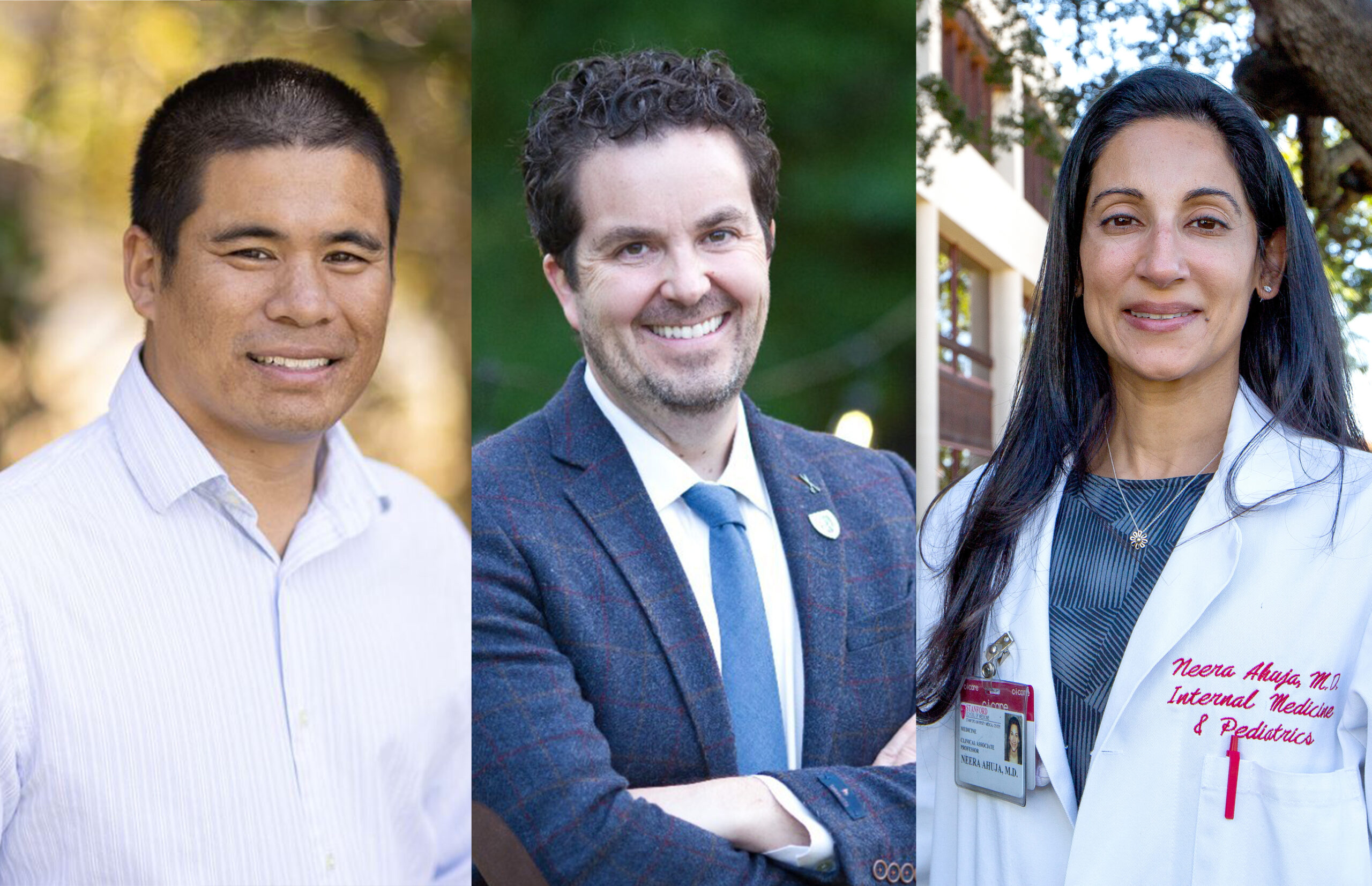
From left: Jeffrey Chi, MD; Tyler Johnson, MD; Neera Ahuja, MD
Hospital Medicine and Oncology Rise to Meet the Needs of More Patients
From left: Jeffrey Chi, MD; Tyler Johnson, MD; Neera Ahuja, MD
Hospital Medicine and Oncology Rise to Meet the Needs of More Patients
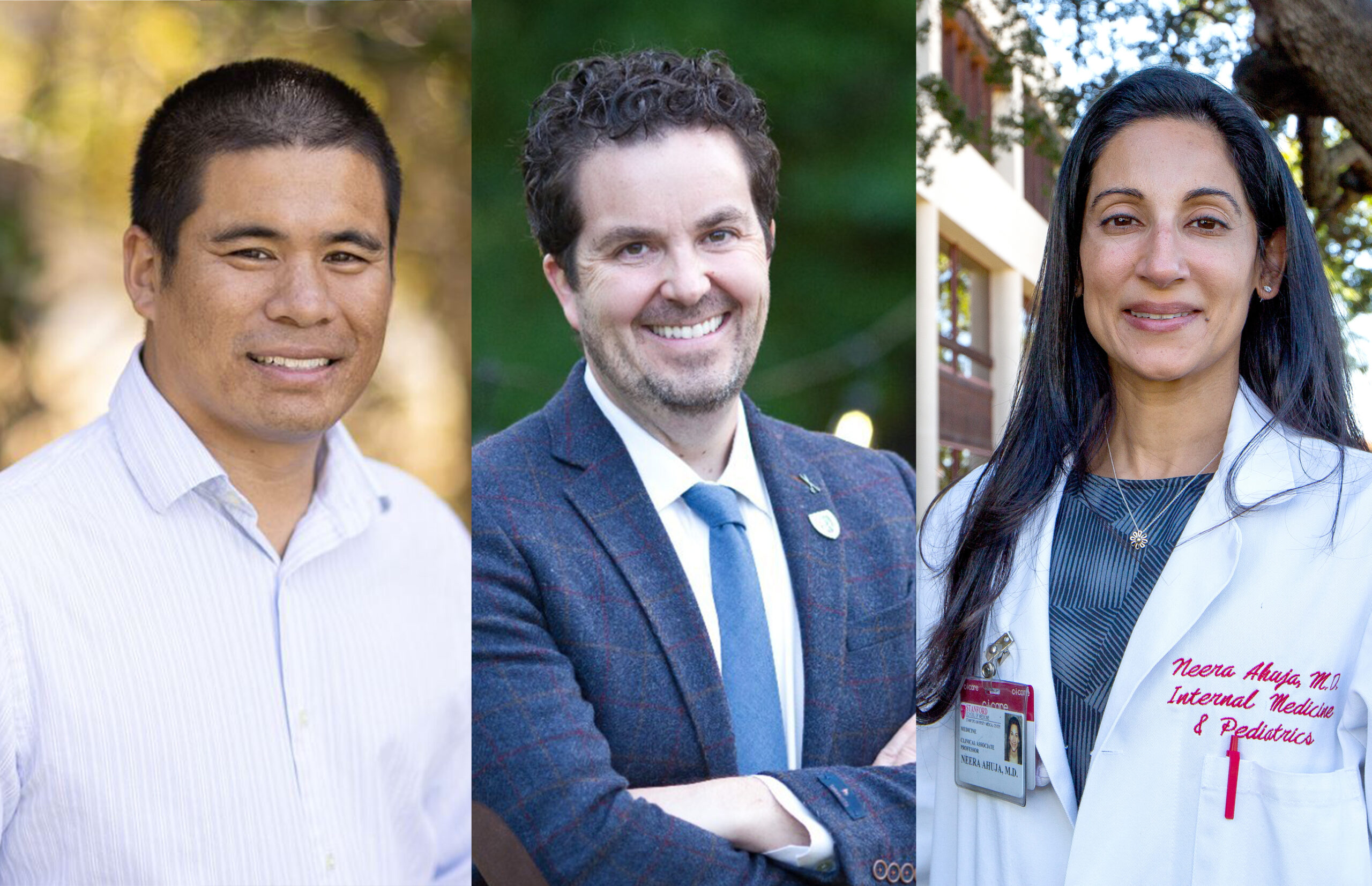
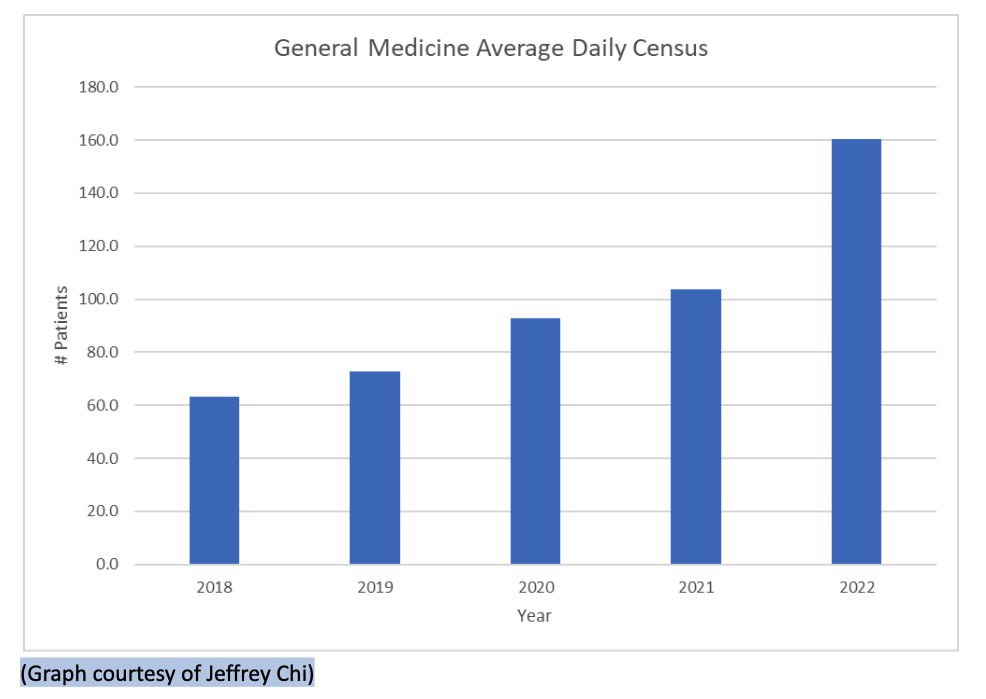
About two years ago, says Tyler Johnson, MD, clinical assistant professor of oncology, the hospital experienced a “perfect storm of events that happened over the course of about six months,” which led to unmanageable numbers of patients relative to the number of health care providers.
Often, in the past, the oncology units experienced occasional high volumes of patients, but internal medicine had always been able to flex up capacity to help in those rare situations. Unfortunately, the increase in patient volumes two years ago was not unique to oncology; internal medicine saw an influx of its own and lacked the capacity to help with patients from other departments. “It became impossible for all of us to provide care for the increasing number of patients, and from the oncology perspective, we no longer had the option of receiving help from other services,” says Johnson.
“There was no contingency in situations of high volume. There was no place for patients to go when the regular services were full,” Johnson recalls.
The excessive and unpredictable volume of new patients started before COVID-19, when Stanford Health Care opened the new hospital at 500 Pasteur Drive. Then, says Neera Ahuja, MD, division chief of hospital medicine, COVID exacerbated the situation.
“During peak portions of the pandemic, the hospital was intermittently filled with COVID patients, and nonemergent procedures and surgeries were canceled or postponed to ensure capacity and safety for patients needing urgent/emergent care. Plus, patients that didn’t have COVID were actually scared to come to the hospital,” she says. Those patients delayed care, which meant that by the time they did return to the hospital, their conditions had often progressed.
“They were a bit sicker, and primary care clinics or specialty clinics were often really full, so for some patients, coming to the ER/hospital was faster,” she adds.
Maintaining high-quality care for all of these patients took a series of Herculean efforts. The hospital needed to renew its strategies and grow its teams.
Click image below to expand
About two years ago, says Tyler Johnson, MD, clinical assistant professor of oncology, the hospital experienced a “perfect storm of events that happened over the course of about six months,” which led to unmanageable numbers of patients relative to the number of health care providers.
Often, in the past, the oncology units experienced occasional high volumes of patients, but internal medicine had always been able to flex up capacity to help in those rare situations. Unfortunately, the increase in patient volumes two years ago was not unique to oncology; internal medicine saw an influx of its own and lacked the capacity to help with patients from other departments. “It became impossible for all of us to provide care for the increasing number of patients, and from the oncology perspective, we no longer had the option of receiving help from other services,” says Johnson.
“There was no contingency in situations of high volume. There was no place for patients to go when the regular services were full,” Johnson recalls.
The excessive and unpredictable volume of new patients started before COVID-19, when Stanford Health Care opened the new hospital at 500 Pasteur Drive. Then, says Neera Ahuja, MD, division chief of hospital medicine, COVID exacerbated the situation.
“During peak portions of the pandemic, the hospital was intermittently filled with COVID patients, and nonemergent procedures and surgeries were canceled or postponed to ensure capacity and safety for patients needing urgent/emergent care. Plus, patients that didn’t have COVID were actually scared to come to the hospital,” she says. Those patients delayed care, which meant that by the time they did return to the hospital, their conditions had often progressed. “They were a bit sicker, and primary care clinics or specialty clinics were often really full, so for some patients, coming to the ER/hospital was faster,” she adds.
Maintaining high-quality care for all of these patients took a series of Herculean efforts. The hospital needed to renew its strategies and grow its teams.
Step 1: Surge Protection
At the start of the influx, “we really needed a solution, more or less right away,” says Johnson. “We created surge services.” Surge services were teams of physicians that were paid per diem to pick up extra shifts and help care for extra patients.
“The standing up of the surge services was a logistical miracle,” says Johnson. “The most challenging aspect of maintaining the surge teams centered around the daily logistics of ensuring constant staffing. Between the days and nights, Rita Pandya, MD, the nocturnist section chief, and myself were, at times, responsible for scheduling up to 16 faculty and trainees per day,” says Jeffrey Chi, MD, section chief of general medicine at hospital medicine, adding that “there was a significant range of experience, ranging from PGY1s to PGY6s, with backgrounds in many specialties.”
The surge teams helped manage the increase in patients while new services like Med12 and LOLA were set up, but since patient loads continued to climb, surge teams have had to continue operating. After two years, explains Chi, the teams have learned a lot about various staffing models. They’ve improved staffing, brought together multiple different specialties, and improved the educational experience for residents.

The standing up of the surge services was a logistical miracle.
— Tyler Johnson, MD, clinical assistant professor of oncology
Step 2: Med12
Between January and July 2022, Heather Wakelee, MD, professor and chief of oncology; Johnson; and their team “advertised, recruited, interviewed, hired, and then got licensed and credentialed, six attending physicians. The new team was developed in just six months, with capacity to care for up to 30 patients a day, which sometimes even went up to 35,” says Johnson.
But the influx of patients continued to grow. Staff had to find even more attending physicians. “We’ve had to increase the number of attendings working at a time from three attendings to five attendings,” says Johnson. “Now, we’re going to have a total of 10 attendings, five on at a time.”
Oncology patients frequently switch between inpatient and outpatient care. Having a dedicated team, dubbed Med12, managing the inpatient care makes communication with the outpatient team more effective, improving the quality of care for the patient.
Med12 team members from left: Jason Chang, MD; Mingwei Yu, MD; Goar Egoryan, MD; Susanna Miao, MD; Margaret Shyu, MD; Koorush Kabiri, MD; and Megha Shalavadi, MD
Step 3: LOLA
As patient volumes continued to grow, the division of hospital medicine created the long length, low acuity (LOLA) service in November 2022. “The physicians were quite busy. And so we thought, ‘What if we take the less sick patients (i.e., low acuity) who still need to be in the hospital … we put them on a special team that just addressed their one need keeping them in the hospital?’ That way, it provided bandwidth for all the other teams to take care of sicker patients more efficiently,” says Ahuja.
Ahuja is extremely proud of the physicians on her team. She says that no matter how tired they were, patient care was “never compromised.” Still, the workload wasn’t sustainable long-term, and the new teams were introduced at just the right time.
“A proxy for a good division is how well you’re able to retain your physicians,” says Ahuja. “And we’ve had excellent retention. This has been successful, and we’ll continue to support our physicians and continue to evolve as times change.”
Step 1: Surge Protection
At the start of the influx, “we really needed a solution, more or less right away,” says Johnson. “We created surge services.” Surge services were teams of physicians that were paid per diem to pick up extra shifts and help care for extra patients.
“The standing up of the surge services was a logistical miracle,” says Johnson. “The most challenging aspect of maintaining the surge teams centered around the daily logistics of ensuring constant staffing. Between the days and nights, Rita Pandya, MD, the nocturnist section chief, and myself were, at times, responsible for scheduling up to 16 faculty and trainees per day,” says Jeffrey Chi, MD, section chief of general medicine at hospital medicine, adding that “there was a significant range of experience, ranging from PGY1s to PGY6s, with backgrounds in many specialties.”
The surge teams helped manage the increase in patients while new services like Med12 and LOLA were set up, but since patient loads continued to climb, surge teams have had to continue operating. After two years, explains Chi, the teams have learned a lot about various staffing models. They’ve improved staffing, brought together multiple different specialties, and improved the educational experience for residents.

The standing up of the surge services was a logistical miracle.
— Tyler Johnson, MD, clinical assistant professor of oncology
Step 2: Med12
Between January and July 2022, Heather Wakelee, MD, professor and chief of oncology; Johnson; and their team “advertised, recruited, interviewed, hired, and then got licensed and credentialed, six attending physicians. The new team was developed in just six months, with capacity to care for up to 30 patients a day, which sometimes even went up to 35,” says Johnson.
But the influx of patients continued to grow. Staff had to find even more attending physicians. “We’ve had to increase the number of attendings working at a time from three attendings to five attendings,” says Johnson. “Now, we’re going to have a total of 10 attendings, five on at a time.”
Oncology patients frequently switch between inpatient and outpatient care. Having a dedicated team, dubbed Med12, managing the inpatient care makes communication with the outpatient team more effective, improving the quality of care for the patient.
Med12 team members from left: Jason Chang, MD; Mingwei Yu, MD; Goar Egoryan, MD; Susanna Miao, MD; Margaret Shyu, MD; Koorush Kabiri, MD; and Megha Shalavadi, MD
Step 3: LOLA
As patient volumes continued to grow, the division of hospital medicine created the long length, low acuity (LOLA) service in November 2022. “The physicians were quite busy. And so we thought, ‘What if we take the less sick patients (i.e., low acuity) who still need to be in the hospital … we put them on a special team that just addressed their one need keeping them in the hospital?’ That way, it provided bandwidth for all the other teams to take care of sicker patients more efficiently,” says Ahuja.
Ahuja is extremely proud of the physicians on her team. She says that no matter how tired they were, patient care was “never compromised.” Still, the workload wasn’t sustainable long-term, and the new teams were introduced at just the right time.
“A proxy for a good division is how well you’re able to retain your physicians,” says Ahuja. “And we’ve had excellent retention. This has been successful, and we’ll continue to support our physicians and continue to evolve as times change.”