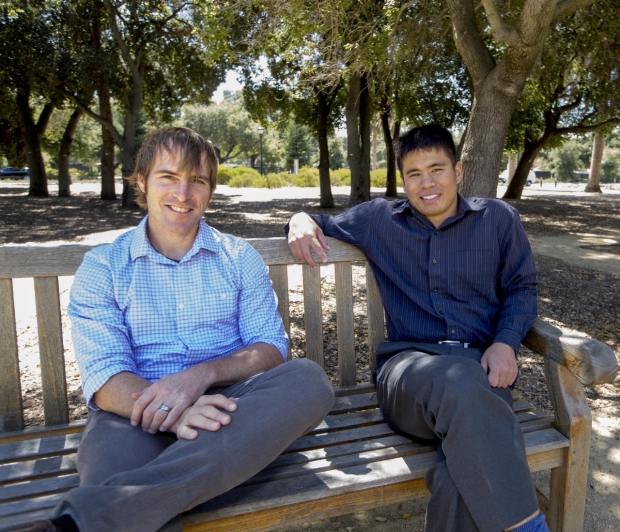
John Kugler, MD, and Jeffrey Chi, MD
Teaching Future Residents
John Kugler, MD, and Jeffrey Chi, MD
Teaching Future Residents
Jeffrey Chi, MD, and John Kugler, MD, have been talking about medical education since they met as interns in 2005, and it’s become the guiding focus of their professional lives. They spend their days in a shared office on the Stanford campus, where they bounce ideas off each other, collaborate on courses and engage in lively discussions.
They’re both drawn to the idea that education — and the commitment to training the next generation — creates confident, comfortable physicians who, in Kugler’s words, are “extremely resilient and well prepared.”
Four years ago, Kugler and Chi, at the behest of then-medical student Vivian Lei, began Stanford’s preparatory education course for senior medical students. The course, titled MD Capstone Experience: Preparation for Residency, provides an introduction to a variety of necessary skills and prepares attendees for the precarious transition from medical student to practicing clinician. During a recent interview, Kugler and Chi, who are both in the division of hospital medicine, discussed the origins of the course and their vision for the future.
Q: You’ve been running the program since 2013. How has the MD Capstone Experience structure — and content — of the class changed over time?
John Kugler: When we started it, we picked three major themes: a clinical skills piece, a clinical knowledge piece and what we were calling advanced communication. Our goal from the beginning was to keep everything practical. For example, these are the things that will keep you from feeling terrible during your first four months of residency.
Jeffrey Chi, MD, and John Kugler, MD, have been talking about medical education since they met as interns in 2005, and it’s become the guiding focus of their professional lives. They spend their days in a shared office on the Stanford campus, where they bounce ideas off each other, collaborate on courses and engage in lively discussions.
They’re both drawn to the idea that education — and the commitment to training the next generation — creates confident, comfortable physicians who, in Kugler’s words, are “extremely resilient and well prepared.”
Four years ago, Kugler and Chi, at the behest of then-medical student Vivian Lei, began Stanford’s preparatory education course for senior medical students. The course, titled MD Capstone Experience: Preparation for Residency, provides an introduction to a variety of necessary skills and prepares attendees for the precarious transition from medical student to practicing clinician. During a recent interview, Kugler and Chi, who are both in the division of hospital medicine, discussed the origins of the course and their vision for the future.
Q: You’ve been running the program since 2013. How has the MD Capstone Experience structure — and content — of the class changed over time?
John Kugler: When we started it, we picked three major themes: a clinical skills piece, a clinical knowledge piece and what we were calling advanced communication. Our goal from the beginning was to keep everything practical. For example, these are the things that will keep you from feeling terrible during your first four months of residency.
We made a few changes the next year: We expanded the course from three days to a full week of class — which went well — and we added in some things like making sure they practiced patient “hand-offs,” which is a big issue in medical education right now.
And this year we’re going to incorporate actual patient experiences. Our students will partner with an intern in the hospital and learn from that person in real time.
Stanford’s MD Capstone Experience course aims to ease the transition from medical student to resident.
Q: Many medical schools have similar capstone courses. What, in your opinion, makes this course unique?
Jeffrey Chi: Other places have graduation courses, but we are lucky to have the resources that we do, which allow us to do more. For example, we wanted to teach students how to respond to pages and how to communicate with nurses, and so we actually assigned them patients that they follow throughout the course. So our students actually draw on things they did the day before and decisions they made previously to influence their future decision making. It’s hard not to have lectures and didactics, but I think the amount of simulated immersion that we are doing is unique.
I would say the emphasis that we have is survival — boot camp. We know that the medical students are smart, we know they can look up almost anything, but this is geared toward your first few months in internship: What are you going to do during that first month or that second month when you are put into a situation when you don’t have the time to sit down at a computer and look stuff up? You are going to call for help, obviously, but what do you do in those first 10 to 15 minutes when nobody’s around, so that you don’t feel like your heart rate is going faster than the patient’s?
Q: As you scale up, what are your visions for the future for this program?
Jeffrey Chi: The course is being considered as a graduate requirement for Stanford School of Medicine students in the near future. So, we’re going to have to scale this to the order of roughly 90 students. Right now we’re getting the word out so people can plan their schedules well in advance. We’ll hopefully learn enough from this year’s course to scale this to an entire class in the next few years.
John Kugler: We may need to offer the class three different times, and we are probably going to cap the numbers in each cohort to about 30 students so they can have a meaningful patient simulation experience. And while we’ve been doing a one-week course, we’d ideally like to move to a two-week course, which we will try for 2017.
We made a few changes the next year: We expanded the course from three days to a full week of class — which went well — and we added in some things like making sure they practiced patient “hand-offs,” which is a big issue in medical education right now.
And this year we’re going to incorporate actual patient experiences. Our students will partner with an intern in the hospital and learn from that person in real time.
Q: Many medical schools have similar capstone courses. What, in your opinion, makes this course unique?
Jeffrey Chi: Other places have graduation courses, but we are lucky to have the resources that we do, which allow us to do more. For example, we wanted to teach students how to respond to pages and how to communicate with nurses, and so we actually assigned them patients that they follow throughout the course. So our students actually draw on things they did the day before and decisions they made previously to influence their future decision making. It’s hard not to have lectures and didactics, but I think the amount of simulated immersion that we are doing is unique.
I would say the emphasis that we have is survival — boot camp. We know that the medical students are smart, we know they can look up almost anything, but this is geared toward your first few months in internship: What are you going to do during that first month or that second month when you are put into a situation when you don’t have the time to sit down at a computer and look stuff up? You are going to call for help, obviously, but what do you do in those first 10 to 15 minutes when nobody’s around, so that you don’t feel like your heart rate is going faster than the patient’s?
Stanford’s MD Capstone Experience course aims to ease the transition from medical student to resident.
Q: As you scale up, what are your visions for the future for this program?
Jeffrey Chi: The course is being considered as a graduate requirement for Stanford School of Medicine students in the near future. So, we’re going to have to scale this to the order of roughly 90 students. Right now we’re getting the word out so people can plan their schedules well in advance. We’ll hopefully learn enough from this year’s course to scale this to an entire class in the next few years.
John Kugler: We may need to offer the class three different times, and we are probably going to cap the numbers in each cohort to about 30 students so they can have a meaningful patient simulation experience. And while we’ve been doing a one-week course, we’d ideally like to move to a two-week course, which we will try for 2017.
