Team Science: Battling Kidney and Heart Diseases
Large Initiatives Evaluate New Treatments for Cardiovascular and Kidney Diseases
Team Science: Battling Kidney and Heart Diseases
Large Initiatives Evaluate New Treatments for Cardiovascular and Kidney Diseases

Glenn Chertow, MD
Physicians are often faced with critically ill patients who have more than one disease, which complicates treatment decisions. A cardiologist who wants to prescribe a diuretic to a patient with high blood pressure, for example, may need to worry about the medication causing kidney damage. So, she consults with the patient’s care team.
Designing and testing new therapies also requires a team, as evidenced by the large team science initiatives being conducted by the Stanford Center for Clinical Research (SCCR). For example, Stanford researchers are collaborating across different sectors (such as academia and industry), institutions, disciplines, and countries to find more effective treatments for kidney and cardiovascular diseases.
“Since early in my career, I saw that the lives of patients with kidney failure are very difficult and their life spans on dialysis are sadly very short. I’ve
spent 30 years trying to improve their treatment and quality of life,” says Glenn Chertow, MD, the Norman S. Coplon/Satellite Healthcare Professor of Medicine in the division of nephrology.
Patients with end-stage kidney disease also have a high risk of cardiovascular disease, but they are typically excluded from studies due to the complexity of their health problems. That’s why Chertow is excited to help launch one of the few randomized clinical trials focused on patients receiving dialysis, he says.
The clinical trial will study the effects of clazakizumab—a monoclonal antibody that reduces inflammation—in patients with kidney failure. Scientists know that inflammation is a contributing cause of cardiovascular disease and that patients on dialysis have exceptionally high rates of both chronic and severe inflammation. So, they hypothesize that using clazakizumab could prolong and improve the quality of these patients’ lives.
After receiving final funding notification from the biopharmaceutical company CSL Behring, the team will begin with a phase 2B trial to figure out the appropriate dose of clazakizumab, followed by a larger phase 3 trial to measure the drug’s effect on patient outcomes.
Chertow and Myles Wolf, MD, chief of nephrology at Duke University School of Medicine, are co-principal investigators of the overall study. Kenneth Mahaffey, MD, professor of cardiovascular medicine and director of SCCR, will serve on the trial’s executive committee.
“Myself, Dr. Mahaffey, and others at SCCR have been involved in the design of the study from day one. It is a real partnership between academics and industry, between Stanford and Duke, and between nephrology and cardiology,” says Chertow. “It shows we actually work together — it’s not siloed to just one institution or one division.”
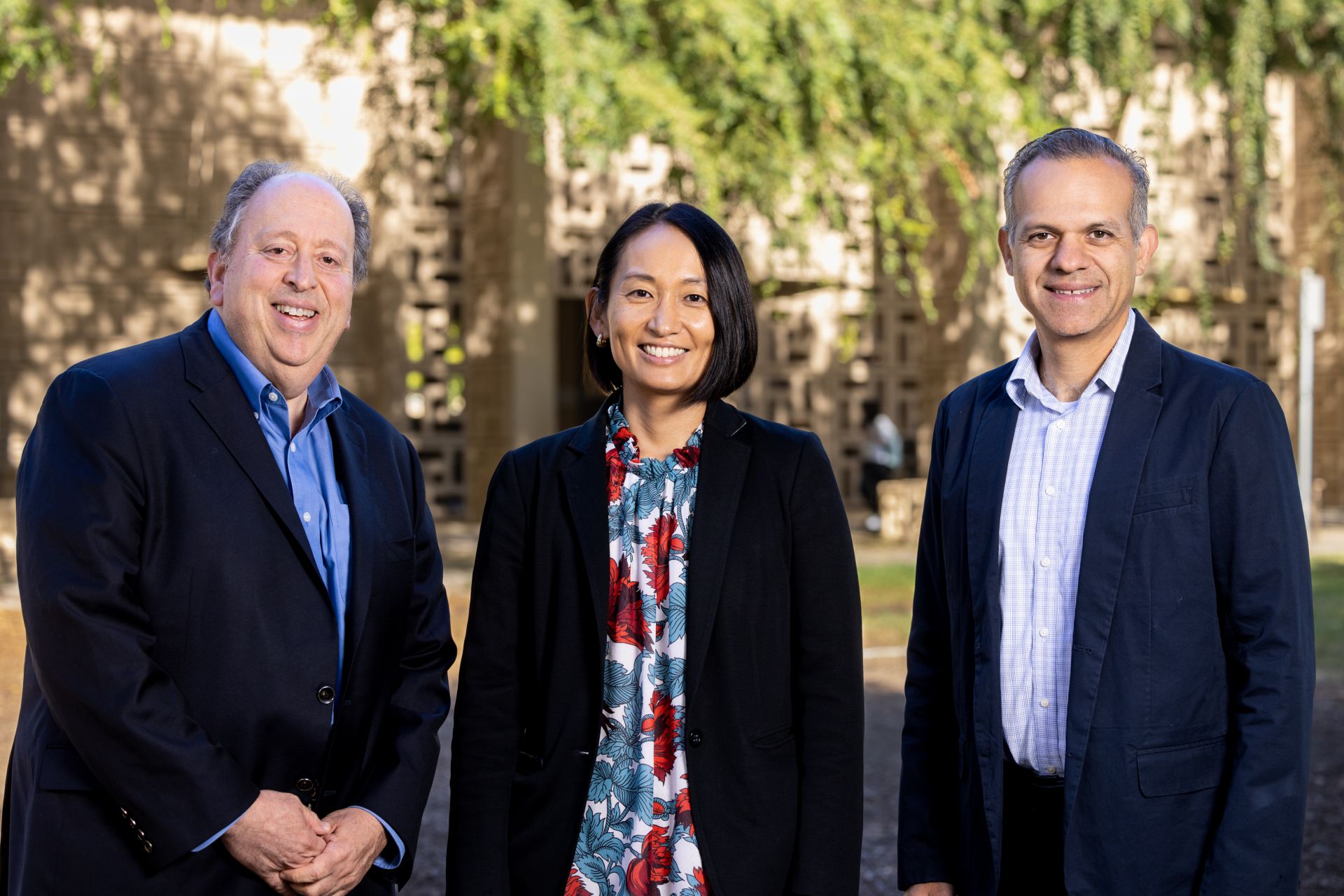
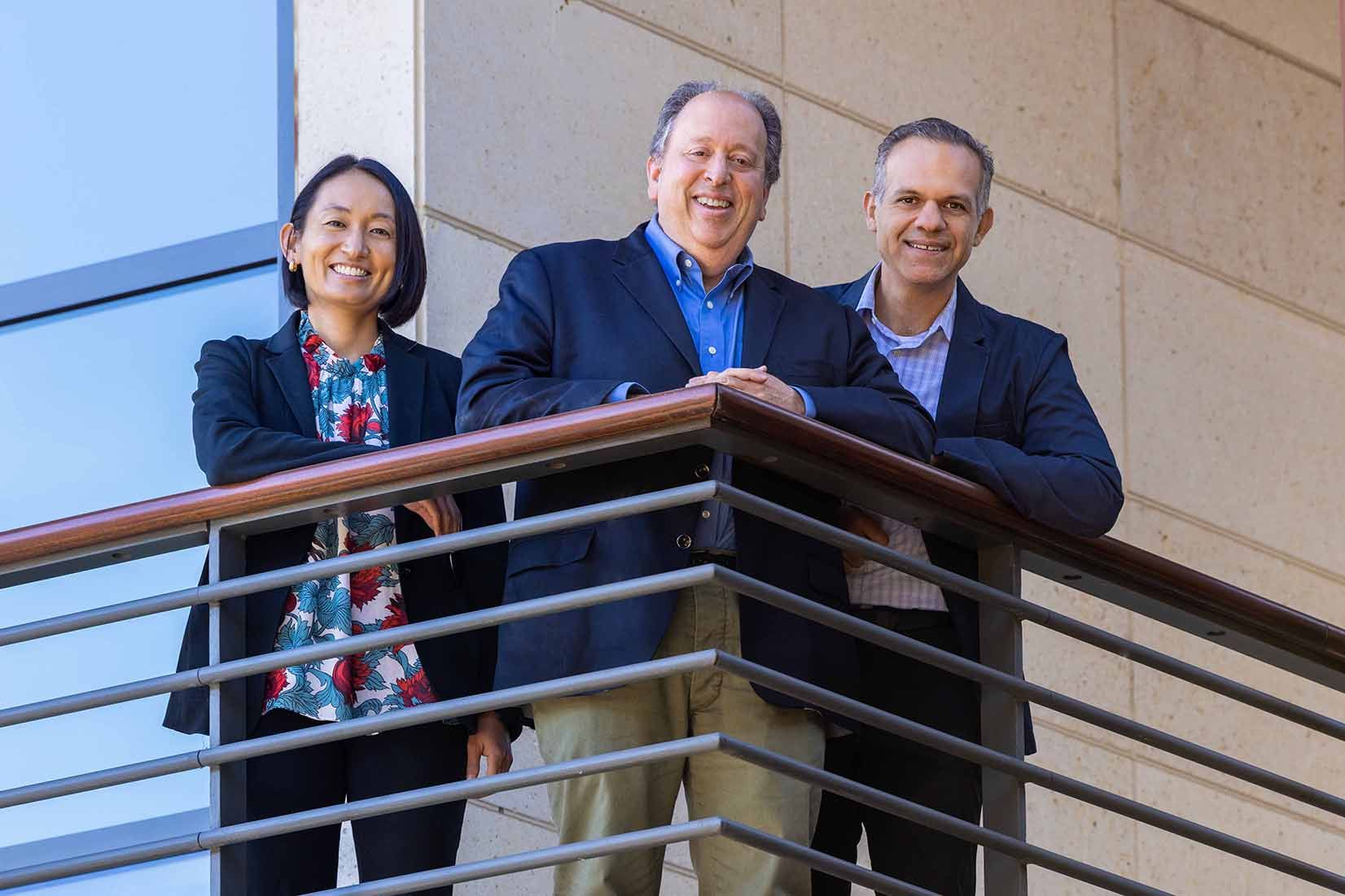
From left: Glenn Chertow, MD; Tara Chang, MD, MS; and Marco Perez, MD.
Patients are dying or suffering miserably from complications of diseases. Finding safe and effective therapies to treat these patients is a motivating force for me every day.
– Kenneth Mahaffey, MD
Patients are dying or suffering miserably from complications of diseases. Finding safe and effective therapies to treat these patients is a motivating force for me every day.
– Kenneth Mahaffey, MD

Marco Perez, MD.
The REACT-AF project represents an academic partnership among Stanford, Johns Hopkins, and Northwestern universities. Rod Passman, MD, professor of cardiology and preventive medicine at Northwestern University’s Feinberg School of Medicine, will oversee the overall initiative, while Mahaffey and Marco Perez, MD, associate professor of cardiovascular medicine, will co-lead Stanford’s efforts.
The faculty bring a lot of clinical and scientific expertise, and the operational research staff understand the regulations, policies, and procedures,” he says. “Together, they create synergies to enhance the design, conduct, and quality of clinical trials.
– Kenneth Mahaffey, MD
The faculty bring a lot of clinical and scientific expertise, and the operational research staff understand the regulations, policies, and procedures,” he says. “Together, they create synergies to enhance the design, conduct, and quality of clinical trials.
– Kenneth Mahaffey, MD

Kenneth Mahaffey, MD

Tara Chang, MD, MS
Collaborating Across Experience Levels
Although led by senior faculty, these large studies will also provide junior faculty, operational staff, and fellows with critical research training.
“Stanford is a learning environment. Dr. Mahaffey and I feel very strongly that we have a responsibility to train the next generation of scientists,” says Chertow. “For example, Dr. Tara Chang, associate professor and chief of nephrology, is a shining example of a physician who completed training at Stanford and is now a national leader at the crossroads of kidney and cardiovascular disease.”
In addition to providing funding and research opportunities, these projects allow Stanford patients to enroll in the studies — a fundamental incentive for the researchers who want to give their patients more options.
“Patients are dying or suffering miserably from complications of diseases,” Mahaffey says. “Finding safe and effective therapies to treat these patients is a motivating force for me every day.”
Team Science Players
CSL Behring study (dialysis patients, clazakizumab):
- Glenn Chertow, MD, the Norman S. Coplon/Satellite Healthcare Professor of Medicine, will co-lead the overall study with Myles Wolf, MD, chief of nephrology at Duke University School of Medicine, in partnership with the biopharmaceutical company CSL Behring and Duke Clinical Research Institute.
- Ken Mahaffey, MD, professor of cardiovascular medicine and director of the Stanford Center for Clinical Research (SCCR), will serve on the trial’s executive committee.
- Tara Chang, MD, associate professor and chief of nephrology, will lead the adjudication committee at Stanford.
NIH REACT-AF study, A-fib study:
The REACT-AF project represents an academic partnership among Stanford, Johns Hopkins, and Northwestern universities.
Rod Passman, MD, professor of cardiology and preventive medicine at Northwestern University’s Feinberg School of Medicine, will oversee the overall initiative, while Ken Mahaffey, MD, professor of cardiovascular medicine and director of the Stanford Center for Clinical Research (SCCR), and Marco Perez, MD, associate professor of cardiovascular medicine, will co-lead Stanford’s efforts along with a team from cardiovascular medicine, the Center for Digital Health, neurology, and SCCR.
