
Joy Wu, MD, PhD, and Aimee Shu, MD
The Contemporary Approach to Managing Bone Disease

Joy Wu, MD, PhD, and Aimee Shu, MD
The Contemporary Approach to Managing Bone Disease
It’s easy enough to take our bones for granted when everything is working correctly. In the normal course of events our bone tissue turns over regularly, with mature bone being replaced (through resorption) by new bone (through formation). Problems arise when our bone strength declines and we sustain fragility fractures.
In the Osteoporosis and Metabolic Bone Disease Clinic and in other venues, Joy Wu, MD, PhD (assistant professor, Endocrinology, Gerontology, & Metabolism) and Aimee Shu, MD (clinical assistant professor, Endocrinology, Gerontology, & Metabolism), see patients with a broad range of problems they are well equipped to manage. And they are increasingly working in a multidisciplinary fashion with colleagues in other divisions and departments.
Osteoporosis
Long considered a disease of aging, particularly of aging women, osteoporosis often first manifests itself as a fragility fracture sustained with minimal trauma. Particularly devastating is the elderly woman who falls and breaks a hip.
Of approximately 250,000 such fractures in the US each year, only 100,000 patients return to normal life; 100,000 are thereafter bedridden and 50,000 die. It is clearly best that osteoporosis be prevented. If that is not possible, the best option is to treat it aggressively once it is diagnosed.
A history of fractures in the young increases the risk of hip fracture later in life. “Among patients who have hip fractures,” Shu says, “more than half had a previous fracture, perhaps of a wrist. So taking care of early fractures and making sure that the patient’s bone health is optimal may help to avoid devastating hip fractures later in life. If you want to build your bones, it’s usually best around the time of your growth spurt for both men and women. We encourage our patients to be playing sports.”
The best known and most used therapies for preventing and treating osteoporosis are the bisphosphonates, which reduce bone resorption.
“This class of drugs has gotten a bad reputation,” Wu explains, “because of two exceedingly rare occurrences associated with them: osteonecrosis of the jaw and atypical femur fractures. But osteonecrosis of the jaw occurs almost entirely in cancer patients, who are treated with much higher doses of bisphosphonates than are patients with osteoporosis, while atypical fractures are clearly associated with longer-term use of bisphosphonates. Our fear is that the rate of hip fractures, which had been declining, will rise if patients abandon these therapies, which are very effective at preventing fragility fractures.”
To avoid atypical fractures from long-term use of bisphosphonates, endocrinologists today employ them with a more nuanced approach. Shu explains that “the evolving concepts are time of therapy initiation, doses used, and duration of treatment – perhaps three to five years – before we take a drug holiday. And then the question becomes: how long a drug holiday do we recommend?”
Osteoporosis is a common problem for women, but men are also at risk. About one-quarter of hip fractures occur in men. Wu says that it’s easy to lose sight of how devastating hip fractures can be for men: “If anything, their mortality rates are even higher than women’s. They are less likely to be treated appropriately yet more likely to die after hip fractures.”
Multidisciplinary Interest in Bone Disease
Diseases of the bones pay no attention to specialty silos. Shu explains that this fact encourages teamwork, “including the relationships that we’ve built with other divisions in the Department of Medicine. For example, we have formed a ‘Bones and Stones’ program with the nephrologists since patients who have abnormally high levels of urine calcium are at higher risk for both kidney stones and low bone mass. We also work closely with our colleagues in rheumatology, oncology, gastroenterology, and of course primary care.”
Important therapies used in rheumatology and oncology (glucocorticoids, for example) can have long-term adverse effects on patients’ bones. Once these patients have survived their acute health threats, they need to attend to their compromised bone health. Shu explains, “We care for childhood survivors of systemic illnesses – leukemia patients and lupus patients, for example – and they often experience bone fragility sooner than their peers do. We strive to be proactive about protecting their bones sooner than when they are in their 80s and 90s.
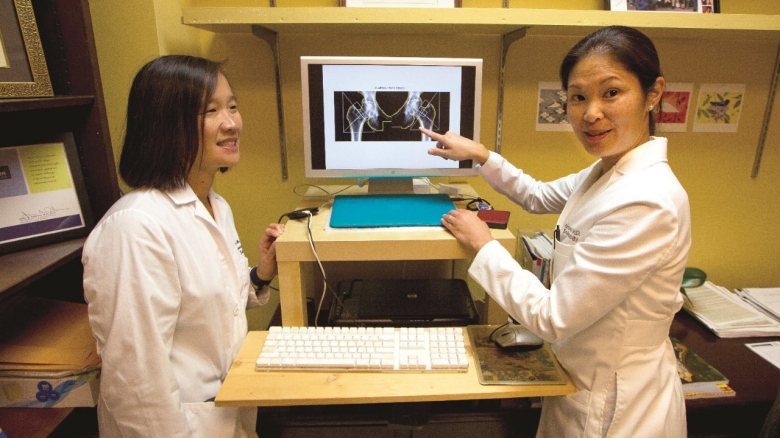
Joy Wu, MD, PhD, and Aimee Shu, MD

We encourage our patients to be playing sports.
It’s easy enough to take our bones for granted when everything is working correctly. In the normal course of events our bone tissue turns over regularly, with mature bone being replaced (through resorption) by new bone (through formation). Problems arise when our bone strength declines and we sustain fragility fractures.
In the Osteoporosis and Metabolic Bone Disease Clinic and in other venues, Joy Wu, MD, PhD (assistant professor, Endocrinology, Gerontology, & Metabolism) and Aimee Shu, MD (clinical assistant professor, Endocrinology, Gerontology, & Metabolism), see patients with a broad range of problems they are well equipped to manage. And they are increasingly working in a multidisciplinary fashion with colleagues in other divisions and departments.
Osteoporosis
Long considered a disease of aging, particularly of aging women, osteoporosis often first manifests itself as a fragility fracture sustained with minimal trauma. Particularly devastating is the elderly woman who falls and breaks a hip. Of approximately 250,000 such fractures in the US each year, only 100,000 patients return to normal life; 100,000 are thereafter bedridden and 50,000 die. It is clearly best that osteoporosis be prevented. If that is not possible, the best option is to treat it aggressively once it is diagnosed.
A history of fractures in the young increases the risk of hip fracture later in life. “Among patients who have hip fractures,” Shu says, “more than half had a previous fracture, perhaps of a wrist. So taking care of early fractures and making sure that the patient’s bone health is optimal may help to avoid devastating hip fractures later in life. If you want to build your bones, it’s usually best around the time of your growth spurt for both men and women. We encourage our patients to be playing sports.”
The best known and most used therapies for preventing and treating osteoporosis are the bisphosphonates, which reduce bone resorption. “This class of drugs has gotten a bad reputation,” Wu explains, “because of two exceedingly rare occurrences associated with them: osteonecrosis of the jaw and atypical femur fractures. But osteonecrosis of the jaw occurs almost entirely in cancer patients, who are treated with much higher doses of bisphosphonates than are patients with osteoporosis, while atypical fractures are clearly associated with longer-term use of bisphosphonates. Our fear is that the rate of hip fractures, which had been declining, will rise if patients abandon these therapies, which are very effective at preventing fragility fractures.”

We encourage our patients to be playing sports.
To avoid atypical fractures from long-term use of bisphosphonates, endocrinologists today employ them with a more nuanced approach. Shu explains that “the evolving concepts are time of therapy initiation, doses used, and duration of treatment – perhaps three to five years – before we take a drug holiday. And then the question becomes: how long a drug holiday do we recommend?”
Osteoporosis is a common problem for women, but men are also at risk. About one-quarter of hip fractures occur in men. Wu says that it’s easy to lose sight of how devastating hip fractures can be for men: “If anything, their mortality rates are even higher than women’s. They are less likely to be treated appropriately yet more likely to die after hip fractures.”
Multidisciplinary Interest in Bone Disease
Diseases of the bones pay no attention to specialty silos. Shu explains that this fact encourages teamwork, “including the relationships that we’ve built with other divisions in the Department of Medicine. For example, we have formed a ‘Bones and Stones’ program with the nephrologists since patients who have abnormally high levels of urine calcium are at higher risk for both kidney stones and low bone mass. We also work closely with our colleagues in rheumatology, oncology, gastroenterology, and of course primary care.”
Important therapies used in rheumatology and oncology (glucocorticoids, for example) can have long-term adverse effects on patients’ bones. Once these patients have survived their acute health threats, they need to attend to their compromised bone health. Shu explains, “We care for childhood survivors of systemic illnesses – leukemia patients and lupus patients, for example – and they often experience bone fragility sooner than their peers do. We strive to be proactive about protecting their bones sooner than when they are in their 80s and 90s.
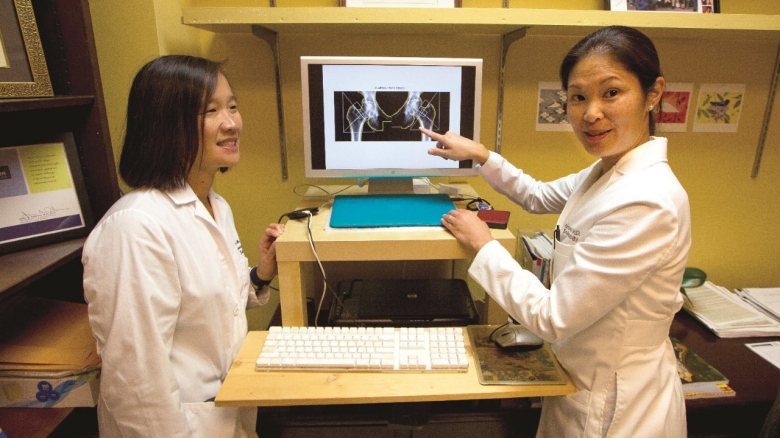
Joy Wu, MD, PhD, and Aimee Shu, MD
“In addition,” Shu continues, “we share many patients with our surgical colleagues in orthopaedics, sports medicine, and transplant medicine. We even have a bone health clinic housed within the orthopaedics facility.”
Novel bone therapies are currently in clinical studies and may debut in coming years. In the meantime, endocrinologists are making use of their current armamentarium in creative combinations and sequences. Wu explains: “There are exciting early studies about how denosumab (FDA-approved in 2010) and teriparatide (approved in 2002) can be used in combination or sequentially. We would consider the combination for patients who have very low bone density or a significant fracture history. Or perhaps for patients who are particularly young and we are concerned about their bones in the future. These are all very early studies so we are just learning.”
Drs. Wu and Shu are encouraged by the many inventive ways they and their colleagues are able to optimize the care of their patients’ bones.
“In addition,” Shu continues, “we share many patients with our surgical colleagues in orthopaedics, sports medicine, and transplant medicine. We even have a bone health clinic housed within the orthopaedics facility.”
Novel bone therapies are currently in clinical studies and may debut in coming years. In the meantime, endocrinologists are making use of their current armamentarium in creative combinations and sequences. Wu explains: “There are exciting early studies about how denosumab (FDA-approved in 2010) and teriparatide (approved in 2002) can be used in combination or sequentially. We would consider the combination for patients who have very low bone density or a significant fracture history. Or perhaps for patients who are particularly young and we are concerned about their bones in the future. These are all very early studies so we are just learning.”
Drs. Wu and Shu are encouraged by the many inventive ways they and their colleagues are able to optimize the care of their patients’ bones.
