Collaboration
2017 Annual Report
 Welcome. Just about a year ago, you received the “2016 Report to Our Community.” Because that was warmly welcomed and often complimented, we undertook another one. Now with a second report in two years, it’s probably safe to refer to these as “annual reports.” I’m happy, therefore, to share our 2017 annual report with you.
Welcome. Just about a year ago, you received the “2016 Report to Our Community.” Because that was warmly welcomed and often complimented, we undertook another one. Now with a second report in two years, it’s probably safe to refer to these as “annual reports.” I’m happy, therefore, to share our 2017 annual report with you.
To select topics to include, I asked the vice chairs, division chiefs and various program heads to make nominations. This resulted in much more to write about than we had space for, so we culled until we reached a representative swath of the department, its people and the many outstanding programs.
Choosing a theme can take some time, but this year collaboration came quickly to mind. We are blessed with ideal geography, which makes it easy to find someone in another division or department or school on campus to work with. We have terrific colleagues to listen to our ideas who often find synergies between what we need and what they do. Collaboration is integral to our makeup.
Glenn Chertow proposed that we write about several members of his nephrology division who are married to Stanford physicians. This became our centerpiece article because it shows how critical continuous collaboration is to running four households, each headed by two doctors.
Several articles focus on the next generation of physicians. Faculty mentoring is one way our trainees learn the value of collaboration in academic research. Some residents take advantage of the Center for Innovation in Global Health’s program to spend a rotation outside the United States. Ten residents are being trained in both internal medicine and anesthesia. The Capstone Experience is a weeklong program for senior medical students to help them make a smooth transition to residency.
Quite a few articles focus on individual researchers. Purvesh Khatri talks about how he explores potential clinical applications of his Big Data discoveries thanks to helpful colleagues with wet labs. Julie Parsonnet praises her research collaborators, while working with undergraduates in her role as a resident fellow in Robinson House – an entirely different level of collaboration. Donna Zulman describes the array of people and services she counts on to help her very high-risk VA patients. Kavitha Ramchandran talks about two different collaborative themes in palliative care.
Haruko Akatsu’s writing about her U.S. medical education evolved into a well-received book and an invitation to help design an innovative medical school curriculum in Japan.
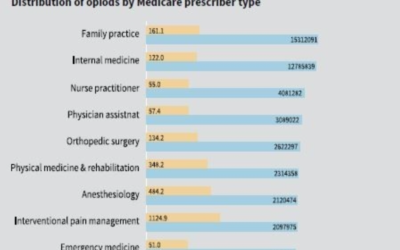
Jason Gotlib’s study of idiopathic hypereosinophilic syndrome began in 2002 with a single patient and progressed through dramatic discoveries, to clinical trials, to successful treatment of patients with other diseases. Walter Park’s research involves a 10-site consortium that researchers expect will help them learn much about diseases of the pancreas. Mark Genovese’s research into inflammatory diseases has been improving options for patients since the 1990s. Crystal Mackall aims to make Stanford a leader in all facets of cell therapy. Mark Nicolls took advantage of the SPARK program to advance a discovery from his lab into clinical trials for pulmonary hypertension. Research from PCOR led by Jonathan Chen shows that over-prescribers of opioids are not just bad actors operating out of backroom pill mills.
Stanford Coordinated Care epitomizes team collaboration overseeing the health of university employees with multiple medical issues. A new master’s degree in community health and prevention research has already stimulated collaborations among several schools and programs on campus. With Presence: The Art and Science of Human Connection, clinicians aim to collaborate among the seven schools on campus to ease the fractious relationship between physicians and technology. The new Center for Digital Health provides opportunities to collaborate with entities in Silicon Valley and elsewhere that crave creative medical input into their processes and products. And Stanford unveils its master of science program for physician assistants.
The collaborative spirit is evident across the spectrum of the Department of Medicine – in our research, when treating patients, with our trainees, overseas and at home, here in Palo Alto.
Sincerely,
Robert Harrington, MD
Chair, Department of Medicine
Department of Medicine in Numbers
Collaboration is a key feature of the Department of Medicine. It is visible at home, in research, treating patients, with trainees, and overseas.
15 Divisions
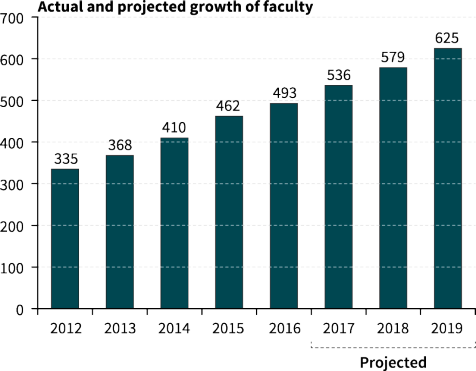
493 Faculty (101 University Tenured and Nontenured Line, 101 Medical Center Line, 264 Clinical Educators, 27 Instructors)
29 Endowed Professors
998 Staff & Research Associates (542 Staff, 95 Research Associates, 361 Temporary Staff)
438 Trainees (125 Residents, 154 MD Fellows, 159 Post-docs)
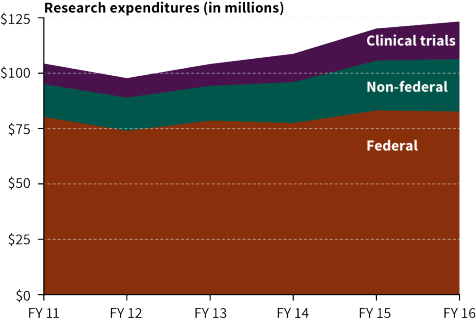
$124M Sponsored Research ($83 million in federal grants, $24 million in non-federal grants, $17 million in clinical grants)
477 Grants (3 Program Projects, 58 R-01s, 35 Ks, 21 Us, 11 Training, 349 Non-Fed & Clinical Trials)
At Home
We write about a faculty member who blurs, blends and ignores a line of demarcation between home and work, and four two-doctor families who strive to find balance between work life and home life. Explore
In Research
Our research topics are numerous and range from repurposing other people’s data to begin to understand immune diseases, to teasing out the possible association between diabetes and cancer of the pancreas, to taking a new therapy for a dread disease from the lab to the clinic. We present a broad effort across Stanford to become a leader in cell therapies for cancer, the inauguration of a new campus resource for capitalizing on digital health tools, and the exposure of the truth about a matter of national concern: overprescribing. Explore
Treating Patients
Here we include articles about ways to improve our care around the world for patients who are dying, and the great success that follows when the care of complex local patients is meticulously coordinated. Veterans who access the VA system have a broad array of services to help them with their physical and mental health care. Two articles tell the story of how a career-long focus on a disease, one in rheumatology and one in hematology, reaps enormous benefits for patients. Finally, Presence: The Art and Science of Human Connection aims to apply campus-wide wisdom to solving the problems that arose when technology imposed itself between the doctor and the patient. Explore
With Trainees
Knowing that our trainees are our future, we celebrate two brand new degree-granting programs: an MS in Physician Assistant Studies and another in Community Health and Prevention Research. We also demonstrate the range of faculty mentors for trainees who have a month in which to do research. Two programs aim to help current and future residents, one designed for those interested in a career in both anesthesiology and internal medicine and the other aimed at easing the transition from learning about doctoring to actually doing it. Explore
Overseas
Our presence beyond the borders of the United States is significant, and two articles explore that vista. Recently, Stanford’s global impact touched communities in Zimbabwe, Borneo and Ecuador. One of our faculty made such an impact on her native Japan that she helped design an innovative curriculum for a new medical school and then joined its faculty. Explore
How We Collaborate
At Home
We write about a faculty member who blurs, blends and ignores a line of demarcation between home and work, and four two-doctor families who strive to find balance between work life and home life.
The Lives and Times of Two-Doctor Families
Dual doctor couples are not a novelty: A 2014 survey by AMA Insurance puts that number at 26 percent for physicians under 40 and at 18 percent for physicians 40 to 59.
A Research Career to Benefit Children and a Life Lived on Campus Among Undergraduates
Julie Parsonnet, MD, professor of infectious diseases and health research and policy, seems most comfortable describing herself as an “enthusiastic citizen of the university.”…
In Research
Our research topics are numerous and range from repurposing other people’s data to begin to understand immune diseases, to teasing out the possible association between diabetes and cancer of the pancreas, to taking a new therapy for a dread disease from the lab to the clinic. We present a broad effort across Stanford to become a leader in cell therapies for cancer, the inauguration of a new campus resource for capitalizing on digital health tools, and the exposure of the truth about a matter of national concern: overprescribing.
Adventures of a Proud Data Parasite
After several career turns, Purvesh Khatri, PhD, assistant professor of medicine (biomedical informatics research–Institute for Immunity, Transplantation and Infection), finds himself a bioinformatician on a quest to improve diagnostics and therapies for infectious diseases.
Riding the Immunotherapy Wave of the Future
Today, most pills dispensed to patients — whether for diabetes, cancer or another disease — are made of synthetic proteins or other lifeless molecules. But in the future, infusions of living cells might become the go-to therapies for many conditions.
Sometimes Diabetes Means Cancer
Walter Park, MD, an assistant professor of gastroenterology & hepatology, acknowledges that it will be many years before he recognizes the fruits of two of his current projects.
The Center for Digital Health Is Open for Business
Recent conversations with architects of the School of Medicine’s new Center for Digital Health painted a picture of how the center will address several questions.
From Bench to Bedside for Pulmonary Hypertension
By collaborating with Stanford’s SPARK program as well as those outside the university, Stanford clinician-scientist Mark Nicolls has moved a drug into clinical trials.
Research Refutes Common Belief about Overprescribing
Researchers with the Center for Primary Care and Outcomes Research (PCOR) have found that prescribing painkillers is widespread among general practitioners.
Treating Patients
Here we include articles about ways to improve our care around the world for patients who are dying, and the great success that follows when the care of complex local patients is meticulously coordinated. Veterans who access the VA system have a broad array of services to help them with their physical and mental health care. Two articles tell the story of how a career-long focus on a disease, one in rheumatology and one in hematology, reaps enormous benefits for patients. Finally, Presence: The Art and Science of Human Connection aims to apply campus-wide wisdom to solving the problems that arose when technology imposed itself between the doctor and the patient.
Improving Palliative Care at Home and Abroad
Improving Palliative Care at Home and Abroad
The Doctor Is Present
It’s a common complaint from contemporary patients: “During routine visits to my doctors, they never make eye contact with me. It feels like we aren’t in the same room.”…
Stanford Coordinated Care Illustrates what Comes from Collaboration
In 2012 Alan Glaseroff, MD, and Ann Lindsay, MD, were recruited to Stanford to develop Stanford Coordinated Care, a clinic for university employees and dependents with multiple medical issues.
From One Patient to the World
A single case during fellowship spurred hematologist Jason Gotlib to develop a drug that’s now helping patients around the world.
Meeting the Challenge of High-risk, Complex Patients in the VA System
Donna Zulman, MD, MS (assistant professor, general medical disciplines), is intrigued by the challenge of caring for patients with multiple medical issues, often exacerbated by mental illness or social stressors.
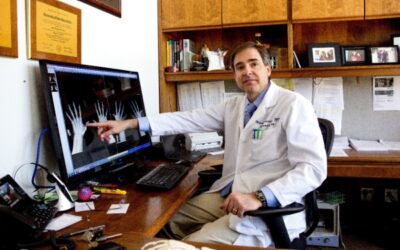
New Days for Rheumatology
Over the past two decades, Mark Genovese, MD, has helped establish Stanford’s bench-to-bedside translational medicine program for chronic inflammatory diseases.
With Trainees
Knowing that our trainees are our future, we celebrate two brand new degree-granting programs: an MS in Physician Assistant Studies and another in Community Health and Prevention Research. We also demonstrate the range of faculty mentors for trainees who have a month in which to do research. Two programs aim to help current and future residents, one designed for those interested in a career in both anesthesiology and internal medicine and the other aimed at easing the transition from learning about doctoring to actually doing it.
Stanford Launches Master of Science Program in Physician Assistant Studies
For the first time, Stanford will offer a master of science program designed to train physician assistants as both clinicians and future leaders in health care.
Newest Degree Program Combines Community Health and Prevention
In fall 2015 the Stanford Prevention Research Center (SPRC) convened an interdisciplinary committee to create a master’s degree anchored in the research and education efforts of SPRC faculty.
Teaching Future Residents
Jeffrey Chi, MD, and John Kugler, MD, have been talking about medical education since they met as interns in 2005, and it’s become the guiding focus of their professional lives.
Stanford Program Trains Half the Nation’s Med-Anesthesia Residents
Stanford offers a unique five-year combined residency training program in internal medicine and anesthesia.
I Have This ‘Research Month.’ What Should I Do with It?
Mindie Nguyen, MD, MAS, is currently mentoring a third-year resident, three second-year residents, and one intern.
Overseas
Our presence beyond the borders of the United States is significant, and two articles explore that vista. Recently, Stanford’s global impact touched communities in Zimbabwe, Borneo and Ecuador. One of our faculty made such an impact on her native Japan that she helped design an innovative curriculum for a new medical school and then joined its faculty.
Working with Limited Resources Teaches Humility in Medicine
Throughout the academic year, many Department of Medicine residents and faculty spend time working overseas or hosting international collaborators on campus.
Across the Pacific
During her medical school days at Brown University and residency at Stanford, Haruko Akatsu, MD, who was born, raised and educated in Japan, got to thinking about the differences between medical education in the two countries.
Connect With Us Online!

In Lasting Memory
With deep regret, we note the passing of Norbert von der Groeben as this report was at press.
Norbert’s remarkable talents are visible in every photograph in this report. Since 2014 he contributed to the Department of Medicine not only through his artistry, but also through his kindness and generosity.
The Department of Medicine will miss him and his warm presence.