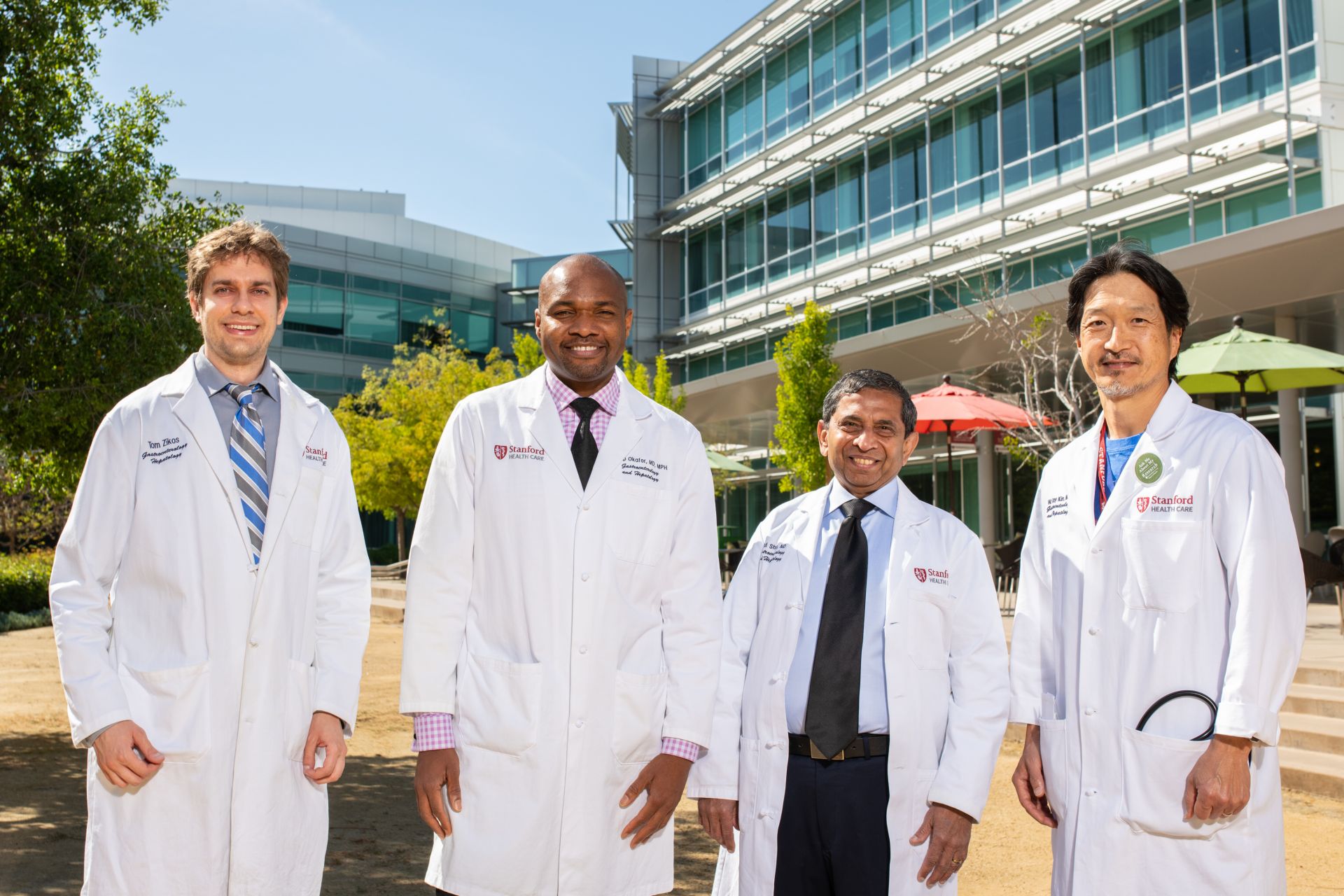
Three Department of Medicine gastroenterologists (Philip Okafor, MD, MPH; Atul Shah, MD, clinical assistant professor; and Thomas Zikos, MD, clinical assistant professor) form the Community GI Group of academic gastroenterologists. These three physicians are dedicated to accepting referrals from the primary care physicians at the Hoover Pavilion. The group works under the direction of the chief of gastroenterology and hepatology, W. Ray Kim, MD.
The mission of the Community GI Group is to speed access and improve communications for both primary care physicians and patients. The group maintains a dedicated inbox on Epic, Stanford Health Care’s electronic medical record system, to support direct communication between gastroenterologists and primary care physicians.
When a primary care physician enters a gastroenterology referral in Epic, he or she can then reach out directly to the Community GI team via the dedicated Epic inbox, if needed. The primary care physician can discuss details about the patient directly with the Community GI team—for instance, if he or she wants tests done before the clinic visit.
In addition to prompt feedback for the primary care physician, the Community GI Group has reserved slots in their clinic schedules to enable them to see urgent referrals.
The system is working to reduce access time and to provide quality care, according to Okafor.
“For example,” he says, “I received a message in our Epic inbox about a primary care physician’s patient who was anemic. I was able to schedule a visit with that patient within days, using one of our reserved scheduling slots. And at the same time, I proactively reserved time for an endoscopy procedure to follow the clinic visit. Within a week, that patient was seen in clinic, underwent their procedure, and had a diagnosis.”