The process of setting up an infrastructure for clinical trials, slow-moving and deeply complicated under normal circumstances, was accelerated with the outbreak of COVID-19. A team of researchers needs to be assembled, patients need to be recruited, and sites need to be established.
But in a matter of weeks, the division of hospital medicine organized an infrastructure at both Stanford Hospital and Stanford Health Care – ValleyCare and implemented Phase 1 of their first trial—to explore the effectiveness of remdesivir—with impressive results.
Neera Ahuja, MD, chief of the division of hospital medicine, was the principal investigator for the global NIH/NIAID Adaptive COVID-19 Treatment Trial (ACTT) at Stanford. The work was greatly facilitated by Kari Nadeau, MD, PhD, the Naddisy Foundation Endowed Professor of Medicine and Pediatrics and hospital medicine’s senior director of clinical research.
Stanford Hospital and SHC – ValleyCare were among the more than 65 sites around the world hosting the ACTT, a randomized, double-blind, placebo-controlled study that included 1,063 patients for its first phase.
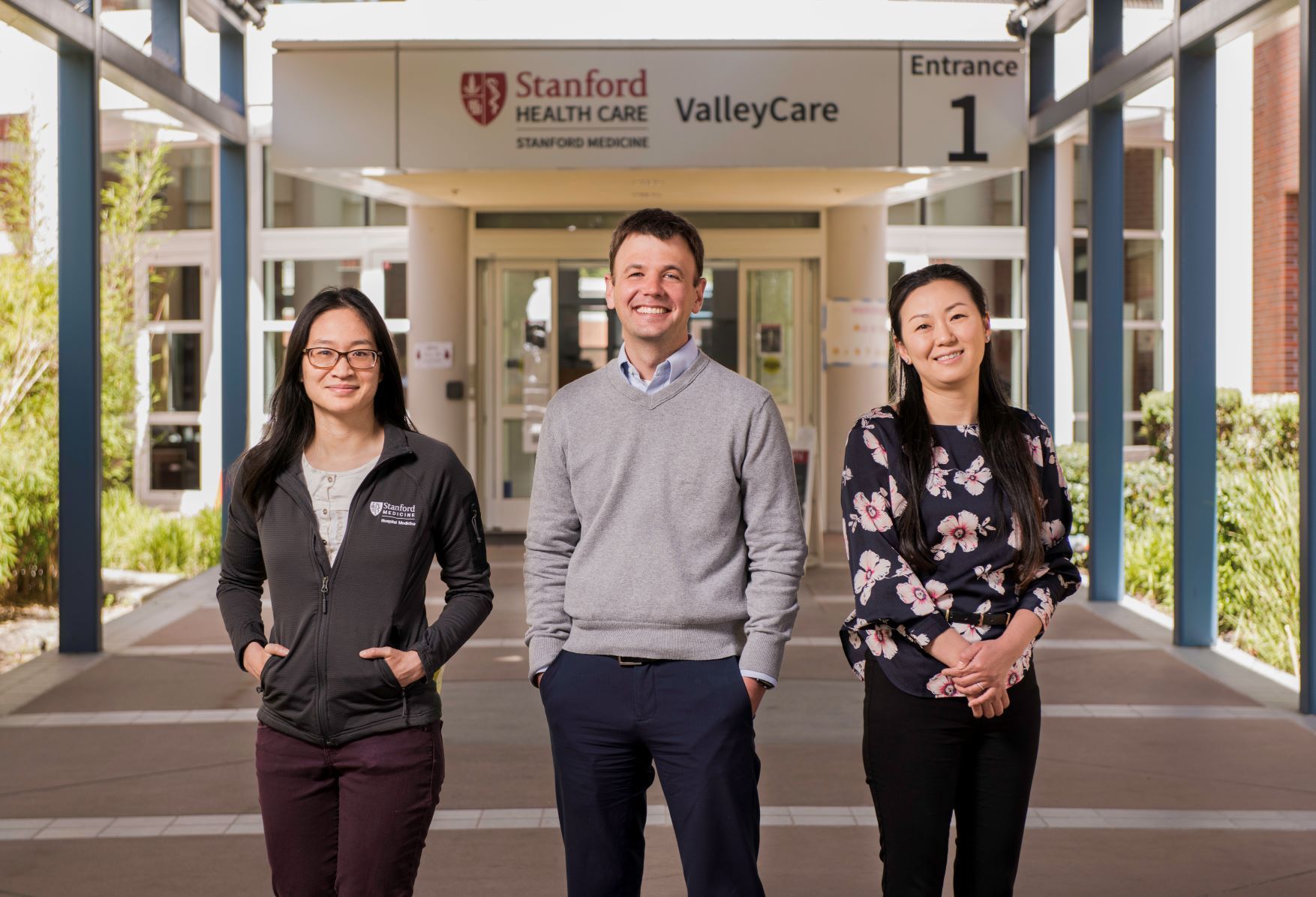
Ahuja and Nadeau worked with clinical associate professor Nidhi Rohatgi, MD, MS; associate professor Sharon Chinthrajah, MD; and clinical assistant professor Rita Pandya, MD, to enroll patients quickly at the Stanford Hospital location. At the other location, David Svec, MD, MBA, clinical associate professor of medicine and chief medical officer at SHC – ValleyCare, was instrumental to the process, along with Minjoung Go, MD, clinical assistant professor of medicine, and Evelyn Ling, MD, MS, clinical assistant professor of medicine and SHC – ValleyCare physician research co-champion.