by dom-wp-admin | Feb 27, 2024 | 2023, Education 2023
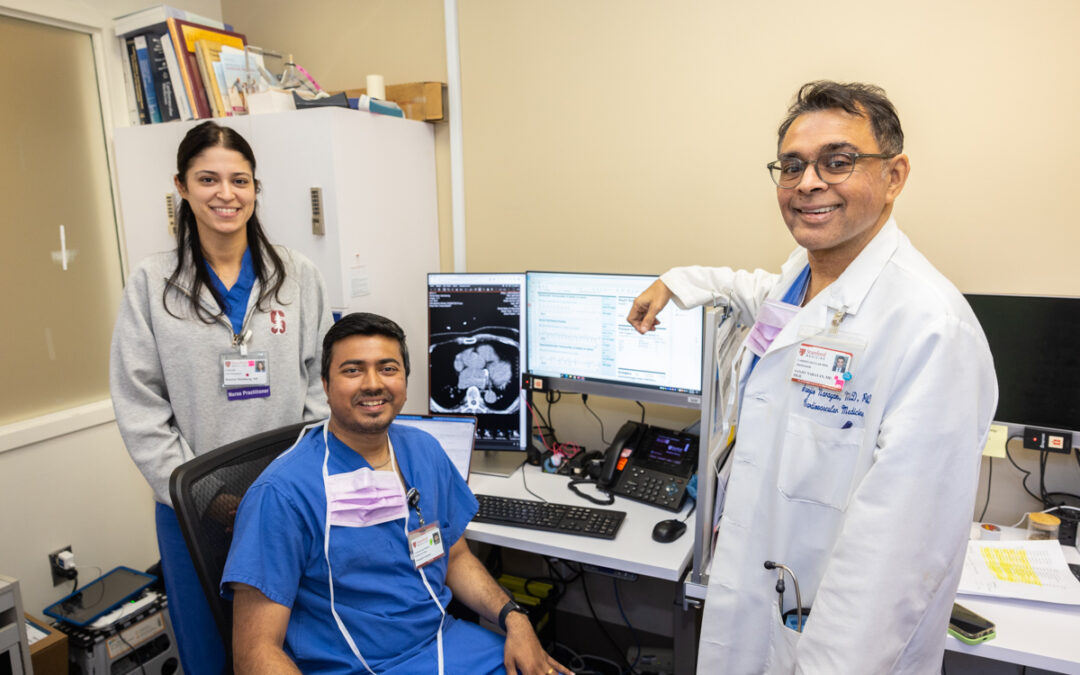
2023 Annual Report Welcome Department by the Numbers All 2023 Stories Credits From left: Desiree Steinberg, NP; Prasanth Ganesan, PhD; and Sanjiv M. Narayan, MD, PhD CHIP: Where Artificial Intelligence and Cardiology Come Together From left: Desiree Steinberg, NP;...

by dom-wp-admin | Feb 27, 2024 | 2023, Rebuilding Community Connections 2023
2023 Annual Report Welcome Department by the Numbers All 2023 Stories Credits Bryan Wu, MD, takes care of a patient at the Cardiovascular Medicine clinic in San Jose, California. Stanford Is Going South New Cardiovascular Clinic Brings Stanford Care to South Bay...