by emli1120 | Feb 26, 2024 | 2016, Elevate the Culture of Clinical Care 2016
Stephanie Harman, MD, and Karl Lorenz, MD, MSHS A Unified Vision for Palliative Care Stephanie Harman, MD, and Karl Lorenz, MD, MSHS A Unified Vision for Palliative Care Just as Stephanie Harman, MD (clinical associate professor, General Medical Disciplines), began...

by emli1120 | Feb 26, 2024 | 2016, Elevate the Culture of Clinical Care 2016
Lauren Cheung, MD, MBA The Future of Primary Care Lauren Cheung, MD, MBA The Future of Primary Care If recent news headlines are any indication, primary care is at a crossroads. A combination of rising health care costs, antiquated care models, increased patient...
by emli1120 | Feb 26, 2024 | 2016, Elevate the Culture of Clinical Care 2016
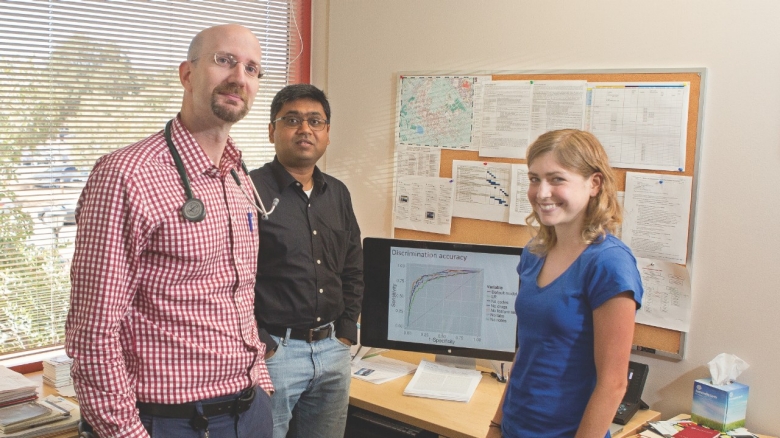
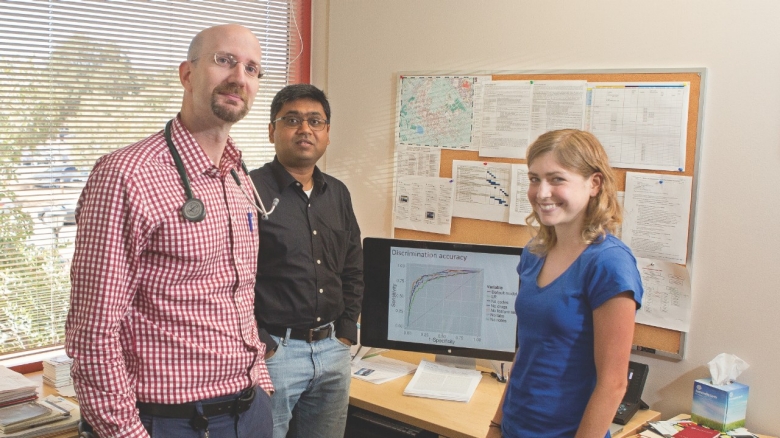
Joshua Knowles, MD, PhD, and Nigam Shah, MBBS, PhD A Good News Story Joshua Knowles, MD, PhD, and Nigam Shah, MBBS, PhD A Good News Story It’s not often that a story contains both good news and an asterisk. This article, about patients with life-threatening familial...

by emli1120 | Feb 26, 2024 | 2016, Elevate the Culture of Clinical Care 2016
Minjoung Go, MD, David Svec, MD, and Brittney Kendall, MHA, BSN,RN Merger of Stanford Health Care and ValleyCare Begins with the Start of a New Hospitalist Program Minjoung Go, MD, David Svec, MD, and Brittney Kendall, MHA, BSN,RN Merger of Stanford Health Care and...

by emli1120 | Feb 26, 2024 | 2016, Elevate the Culture of Clinical Care 2016
Joy Wu, MD, PhD, and Aimee Shu, MD The Contemporary Approach to Managing Bone Disease Joy Wu, MD, PhD, and Aimee Shu, MD The Contemporary Approach to Managing Bone Disease It’s easy enough to take our bones for granted when everything is working correctly. In the...