by dom-wp-admin | Feb 27, 2024 | 2023, Research 2023
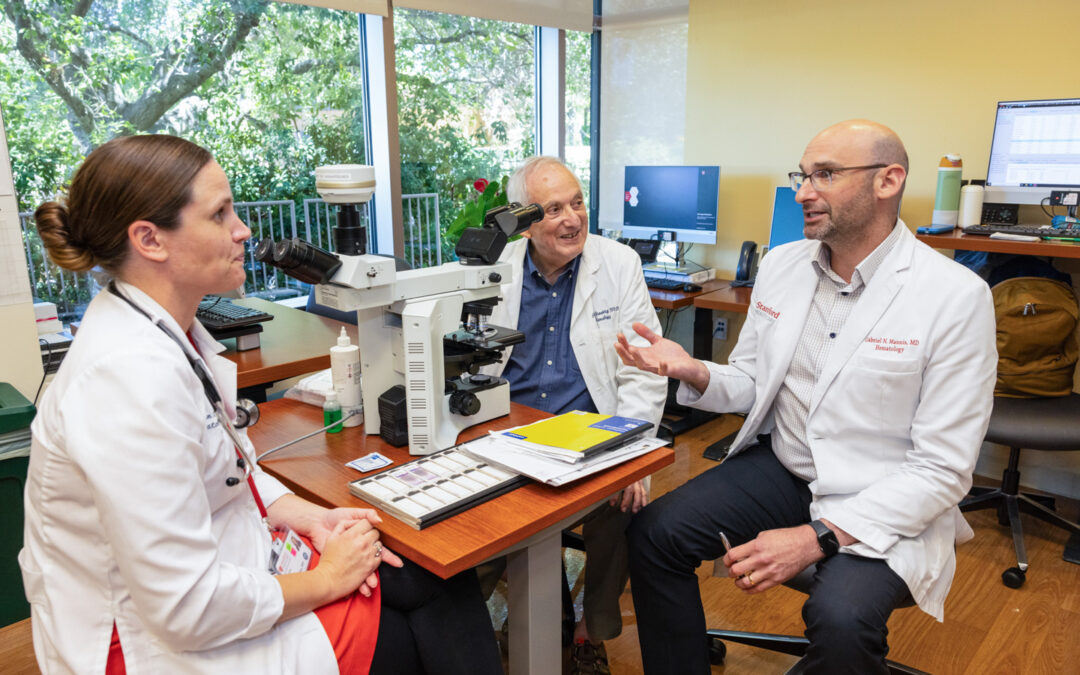
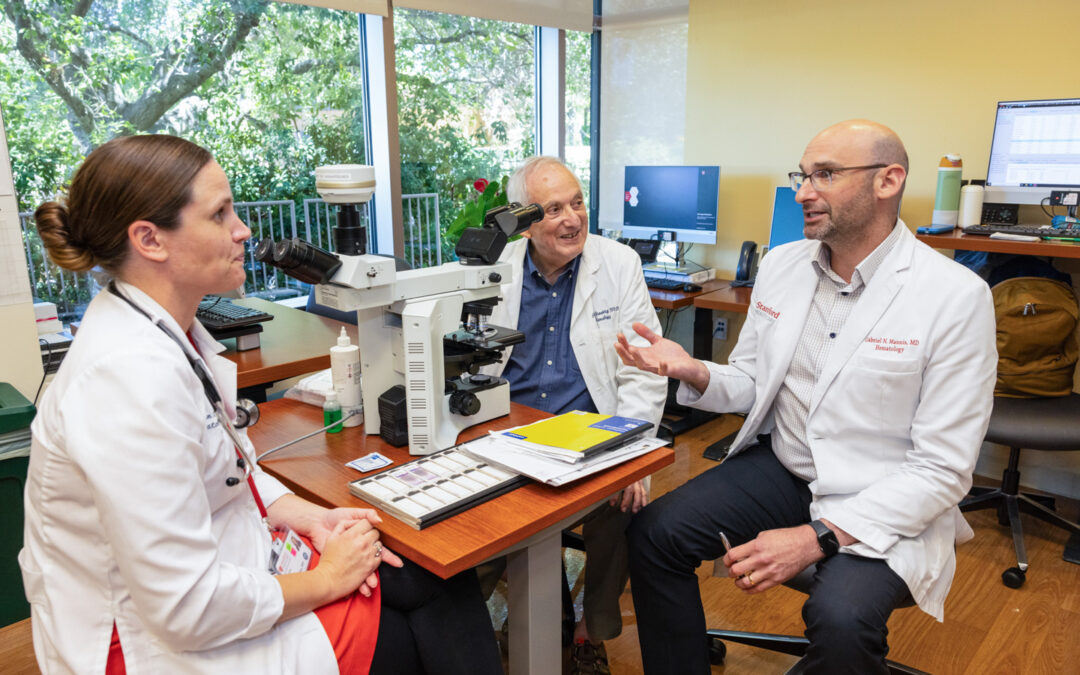
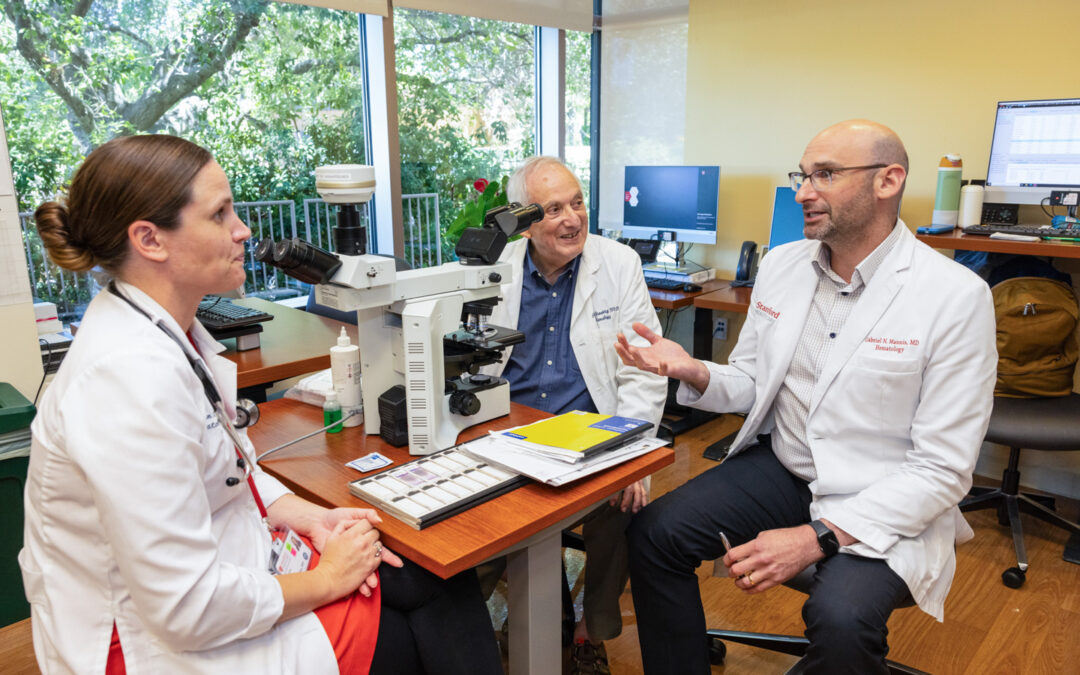
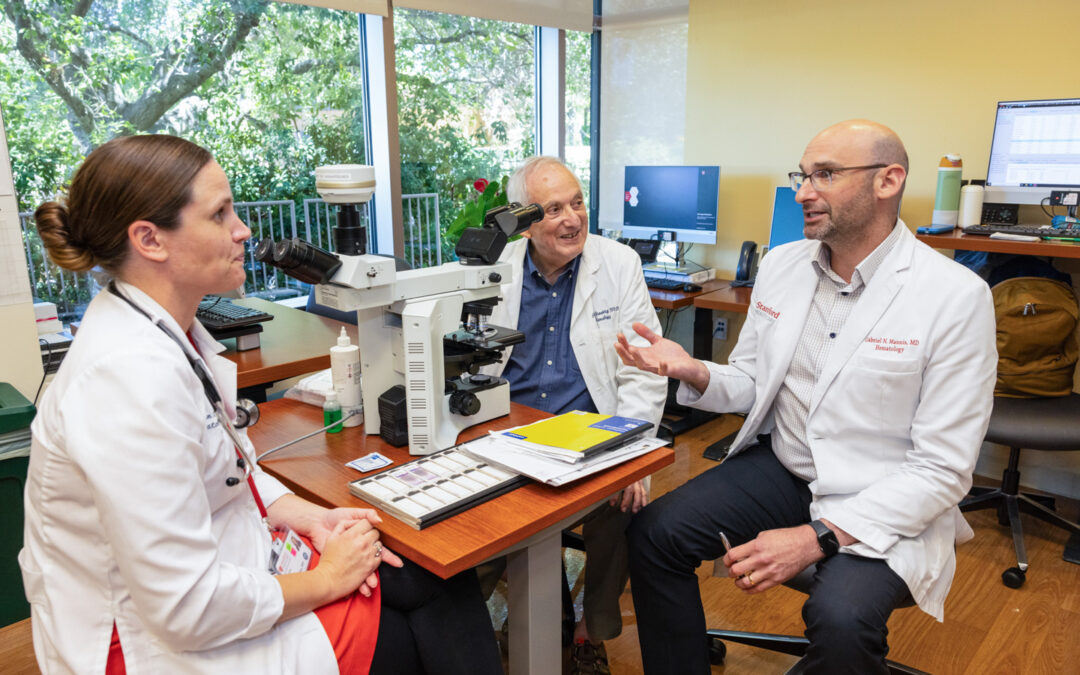
2023 Annual Report Welcome Department by the Numbers All 2023 Stories Credits From left: Cailin Collins, MD, Peter Greenberg, MD, and Gabe Mannis, MD On the Hunt for Knowledge Two Hematologists, Two Challenging Diseases, Two Careers Dedicated to the Pursuit of Answers...

by dom-wp-admin | Feb 27, 2024 | 2023, Education 2023
2023 Annual Report Welcome Department by the Numbers All 2023 Stories Credits Michaela Kiernan, PhD How to Secure Competitive R01 Research Grants? Check Out This Program! Michaela Kiernan, PhD How to Secure Competitive R01 Research Grants? Check Out This Program! One...